Chapter 1: Overview of the Endocrine System
3. Types and Mechanisms of Hormonal Action
3.2. Mechanisms of Action
Hormones act by binding to specific receptors and triggering a biological response. The mechanism depends on the hormone type:
1. Recetors
1.1 Membrane Receptor Mechanism (for Water-Soluble Hormones)
- Receptor location: Cell surface.
- Receptor types:
- Direct effects on membrane ion channels (surface receptors)
- Direct activation of intracellular enzymes (surface receptors)
- Activation of G proteins/second messenger system (surface receptors)
- Direct activation of specific genes (intracellular receptors).
Note: A certain receptor type may be present in 100 – 1,000,000 copies on a single cell.
- Mechanism:
- Hormone binds to receptor → activates second messenger system (e.g., cAMP, IP₃/DAG).
- Second messengers amplify the signal inside the cell.
- Examples: Insulin, adrenaline.
1.2. Intracellular Receptor Mechanism (for Lipid-Soluble Hormones)
- Receptor location: Cytoplasm or nucleus.
- Mechanism:
- Hormone enters cell → binds intracellular receptor → hormone-receptor complex binds DNA → regulates gene expression (transcription).
- Examples: Cortisol, thyroid hormones
2. Signal Transduction Pathways
- Once the chemical signal has been detected by the receptor it must be converted, or transduced, to a form that is meaningful to the cell's metabolic machinery.
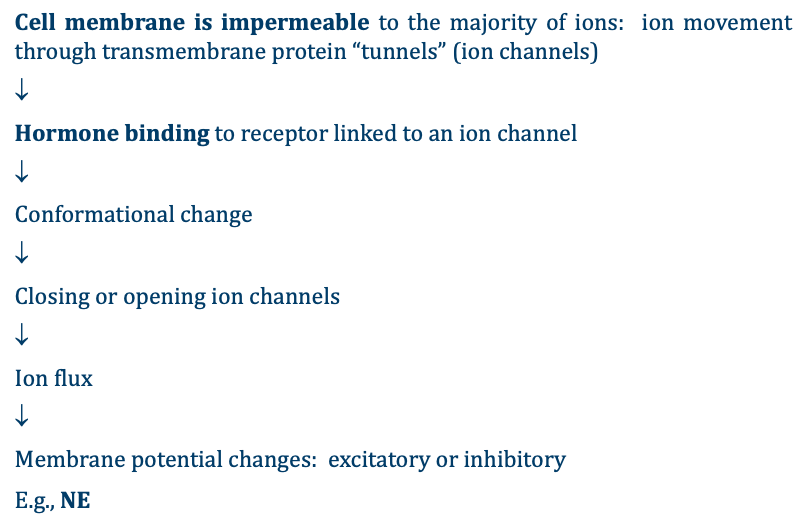
- Binding of hormones to cell surface receptors initiate the closing or opening of ion channels (affecting the permeability of the cell membrane) or initiate a signaling cascade that is carried out by a molecule called a second messenger. In this case, the hormone is called a first messenger.
- Common second messenger systems:
- ion channel‑linked receptors
- cAMP (cyclic AMP) – activates protein kinase A.
- IP₃/DAG (inositol triphosphate/diacylglycerol) – increases intracellular calcium.
- Activation of specific genes
2.1 Pathways Involving Cell Membrane Hormone Receptors
A. ion channel‑linked receptors
B. Enzyme-Linked Receptors (the second messenger pathway)
- Intracellular moiety itself has enzymatic activity or is associated directly with intracellular enzymes → the enzyme produces intra-cellular messengers (called “second messengers”).
- A second messenger in the cytoplasm is required bring about the change in metabolism (the hormone is the first messenger but it never enters the cell).
- The second messenger used by most hormones is cyclic adenosine monophosphate (cAMP).
- In the cAMP second messenger system, a water-soluble hormone binds to its receptor in the cell membrane ((Step 1 in Figure below)
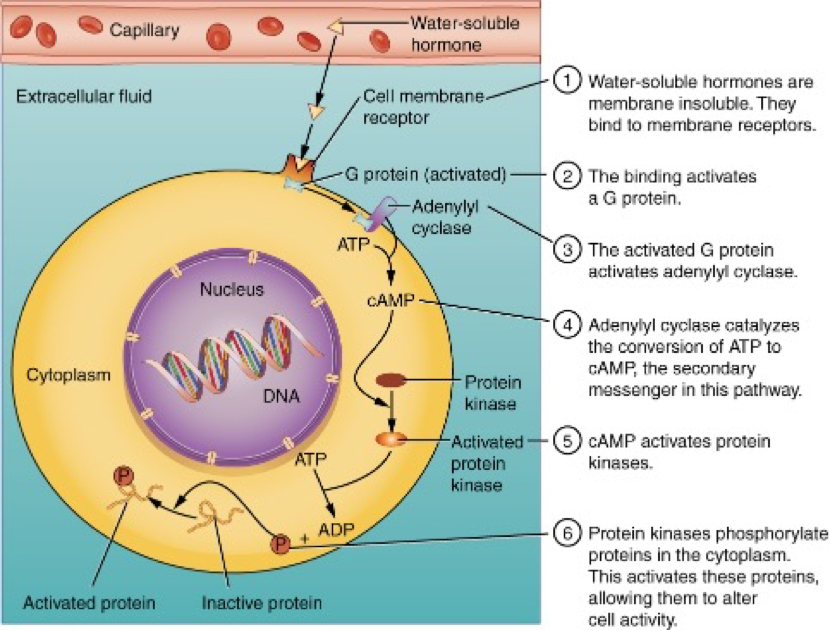
- This receptor is associated with special membrane proteins called G protein, and binding of the hormone activates the G-protein component (Step 2).
- G proteins act as “middlemen” between receptor and second messenger.
- The activated G protein in turn activates an enzyme called adenylyl cyclase, also known as adenylate cyclase (Step 3), which converts adenosine triphosphate (ATP) to cAMP (Step 4).
- As the second messenger, cAMP activates a type of enzyme called a protein kinase that is present in the cytosol (Step 5).
- Activated protein kinases initiate a phosphorylation cascade, in which multiple protein kinases phosphorylate (add a phosphate group to) numerous and various cellular proteins, including other enzymes (Step 6).
- The phosphorylation of cellular proteins can
trigger a wide variety of effects, from nutrient metabolism to the synthesis of
different hormones and other products.
- e.g., cAMP activates protein kinase, which activates phosphorylase kinase, which activates glucose phosphorylase which hydrolyzes glycogen.
- The effects vary according to the type of target cell, the G proteins and kinases involved, and the phosphorylation of proteins
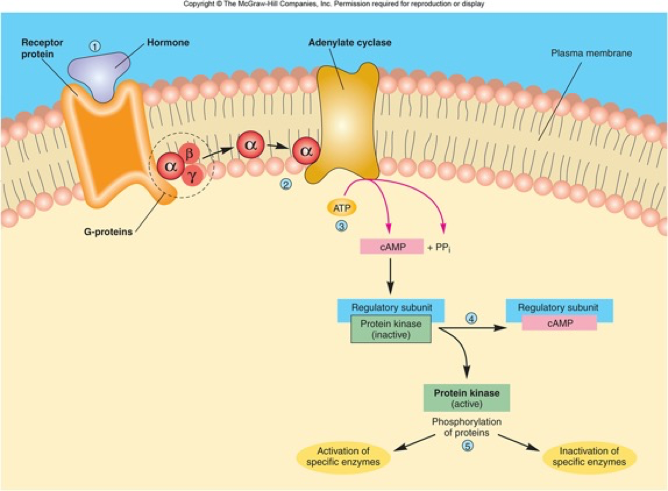
- Examples of hormones that use cAMP as a second messenger include calcitonin, which is important for bone construction and regulating blood calcium levels; glucagon, which plays a role in blood glucose levels; and thyroid-stimulating hormone, which causes the release of T3 and T4 from the thyroid gland.
- Importantly, there are also G proteins that decrease the levels of cAMP in the cell in response to hormone binding. For example, when growth hormone–inhibiting hormone (GHIH), also known as somatostatin, binds to its receptors in the pituitary gland, the level of cAMP decreases, thereby inhibiting the secretion of human growth hormone.
- Not all water-soluble hormones initiate the cAMP second messenger system. One common alternative system uses calcium ions as a second messenger.
- In this system, G proteins activate the enzyme phospholipase C (PLC), which functions similarly to adenylyl cyclase.
- Once activated, PLC cleaves a
membrane-bound phospholipid into two molecules:
- diacylglycerol (DAG) and
- inositol triphosphate (IP3)
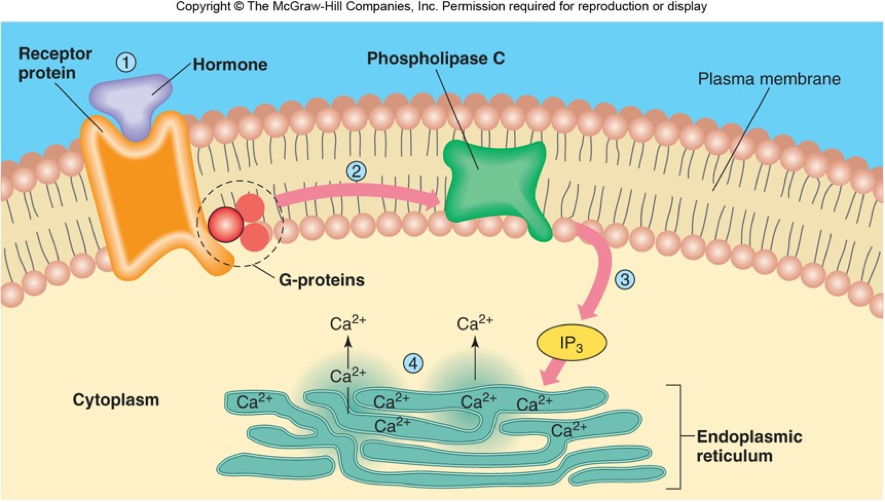
- Like cAMP, DAG activates protein kinases that initiate a phosphorylation cascade. At the same time, IP3 causes calcium ions to be released from storage sites within the cytosol, such as from within the smooth endoplasmic reticulum.
- The calcium ions then act as second messengers in two ways: they can influence enzymatic and other cellular activities directly, or they can bind to calcium-binding proteins, the most common of which is calmodulin.
- Upon binding calcium, calmodulin is able to modulate protein kinase within the cell.
- Examples of hormones that use calcium ions as a second messenger system include angiotensin II, which helps regulate blood pressure through vasoconstriction, and growth hormone–releasing hormone (GHRH), which causes the pituitary gland to release growth hormones.
2.2 Pathways Involving Intracellular Hormone Receptors (Direct gene activation)
§ These hormones are mostly synthesized from cholesterol. These include hormones for sex (estrogen, progesterone, testerone), thyroid and renal (aldosterone) function.
§ These are produced in one cell, then are released into the blood, circulate to all cells, and then permeate across the plasma membrane (due to their lipid solubility) to bind to receptors in the cytosol or nucleus (see step 1 and 2 in Fig below)

- § After binding to the home binding
domain on the receptor, the hormone + receptor complextranslocate to
the nucleus and bind to a
particular sequence of DNA (hormone response element or HRE) in a gene,
which then becomes activated DNA (step 3).
- HRE sites of specific genes, e.g., estrogen-response element; progesterone-response element; etc
- For both steroid and thyroid hormones, binding of the hormone-receptor complex with DNA triggers transcription of a target gene to mRNA (step 4), which moves to the cytosol where it directs protein synthesis by ribosomes (step 5).
- Example
- Low blood [Na] triggers cells in the adrenal cortex to release aldosterone into the blood stream.
- This steroid hormone then circulates throughout the body and binds to receptors in the cytosol of cells in the kidney and gastrointestinal tract.
- The receptor + aldosterone complex moves into the nucleus, where it activates two genes, one for the Na/K-pump and a second for a Na channel.
- These new proteins are inserted into the plasma membranes of the GI and renal cells, leading to increased entry of Na into the cells (through the channels) and increased pumping of Na out of the cells into the blood stream (on the Na/K-pump).
- This increases uptake of Na from the gut and increases Na retention by the kidneys, which increases blood [Na], returning the body to the correct [Na]
- Due to the fact that all this takes time and proteins are produced, steroid hormones generally are longer acting, both in terms of the time it takes to activate the changes in cell functions and also in terms of how long the new protein will act: over hours or even days.
- The final step is the desired metabolic response.
- The response may include the stimulation of protein synthesis, activation or deactivation of enzymes, alteration in the permeability of the cell membrane, altered rates of mitosis and cell growth, and stimulation of the secretion of products.
- Moreover, a single hormone may be capable of inducing different responses in a given cell.
Cellular Response to Hormones: