Hypothalamus and Pituitary Gland
| Site: | Newgate University Minna - Elearning Platform |
| Course: | Endocrine and Reproductive System |
| Book: | Hypothalamus and Pituitary Gland |
| Printed by: | Guest user |
| Date: | Thursday, 8 January 2026, 1:22 AM |
Description
Learning Objectives:
- Describe the location and anatomy of the hypothalamus and pituitary.
- Explain the functional relationship between the two structures.
1. Introduction to the Hypothalamus
- The hypothalamus is a small but critically important part of the brain that plays a central role in maintaining homeostasis by integrating autonomic, endocrine, and behavioral responses.
- Despite its small size (about 4 g), it influences nearly every system in the body, including temperature regulation, hunger, thirst, sleep–wake cycles, emotional behavior, and hormonal secretion via the pituitary gland.
Location and Anatomical Boundaries
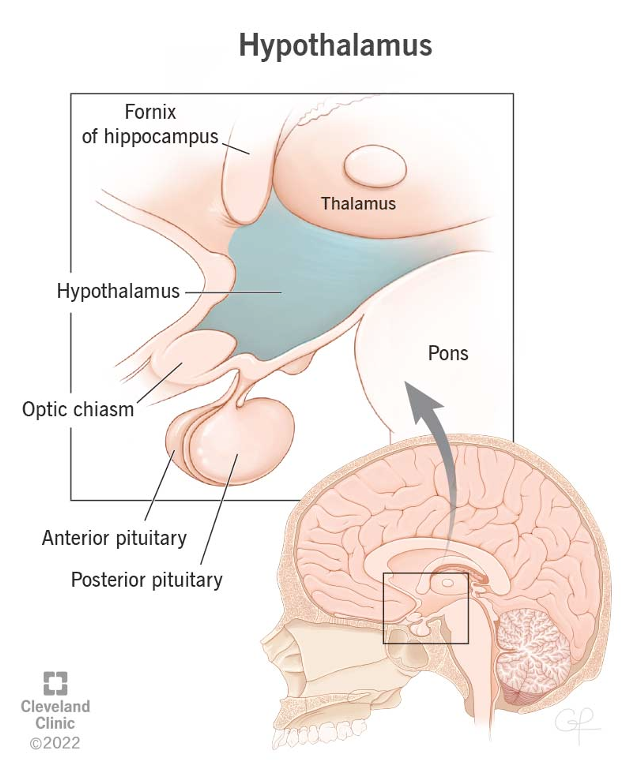
The hypothalamus is located below the thalamus and forms the floor and part of the walls of the third ventricle.
- Superior (Above): Thalamus
- Inferior (Below): Extends to the base of the brain; bounded by the optic chiasm, infundibulum, and mammillary bodies
- Anterior: Optic chiasm and lamina terminalis
- Posterior: Midbrain tegmentum
- Lateral: Internal capsule and subthalamic region
- Medial: Third ventricle
Surface landmarks:
- Optic chiasm: Anterior to the hypothalamus
- Infundibulum (pituitary stalk): Connects hypothalamus to pituitary gland
- Mammillary bodies: Paired rounded structures marking the posterior limi
Subdivisions of the Hypothalamus
For descriptive purposes, the hypothalamus is divided into three anteroposterior regions and three mediolateral zones:
A. Anteroposterior Regions
1. Anterior (Chiasmatic) Region:
- Located above the optic chiasm
- Includes the supraoptic, paraventricular, preoptic, and suprachiasmatic nuclei
2. Tuberal (Middle) Region:
- Located above the tuber cinereum and infundibulum
- Includes the arcuate, ventromedial, and dorsomedial nuclei
3. Posterior (Mammillary) Region:
- Located above and behind the mammillary bodies
- Includes the posterior nucleus and mammillary nuclei
B. Mediolateral Zones
- Periventricular Zone: Thin strip along the third ventricle; contains neurons regulating endocrine functions
- Medial Zone: Contains most hypothalamic nuclei; involved in integrating autonomic and endocrine responses
- Lateral Zone: Contains medial forebrain bundle and scattered nuclei; involved in feeding and arousal
1.1. Major Hypothalamic Nuclei and Their Functions
Below is a summary of key hypothalamic nuclei, their locations, and functions:
|
Nucleus |
Region |
Main Functions |
|
Supraoptic |
Anterior |
Produces antidiuretic hormone (ADH) → transported to posterior pituitary |
|
Paraventricular |
Anterior |
Produces oxytocin and some ADH; regulates stress, metabolism, lactation |
|
Preoptic (Medial & Lateral) |
Anterior |
Thermoregulation (heat loss), sexual behavior, gonadotropin regulation |
|
Suprachiasmatic |
Anterior |
Biological clock – controls circadian rhythms via retinal input |
|
Arcuate |
Tuberal |
Regulates secretion of pituitary hormones via releasing/inhibiting hormones; involved in feeding |
|
Ventromedial |
Tuberal |
Satiety center – inhibits feeding; stimulation → stop eating |
|
Dorsomedial |
Tuberal |
Emotional behavior, autonomic regulation |
|
Posterior nucleus |
Posterior |
Heat conservation, sympathetic responses, arousal |
|
Mammillary nuclei |
Posterior |
Part of limbic system; involved in memory and learning via mammillothalamic tract |
1.2. Functions of the Hypothalamus
The hypothalamus serves as the control center linking the nervous system and endocrine system. Its major functions include:
1. Autonomic Nervous System Regulation
- Controls sympathetic and parasympathetic activity
- Influences heart rate, blood pressure, gastrointestinal motility, pupil size, sweating, and thermoregulation
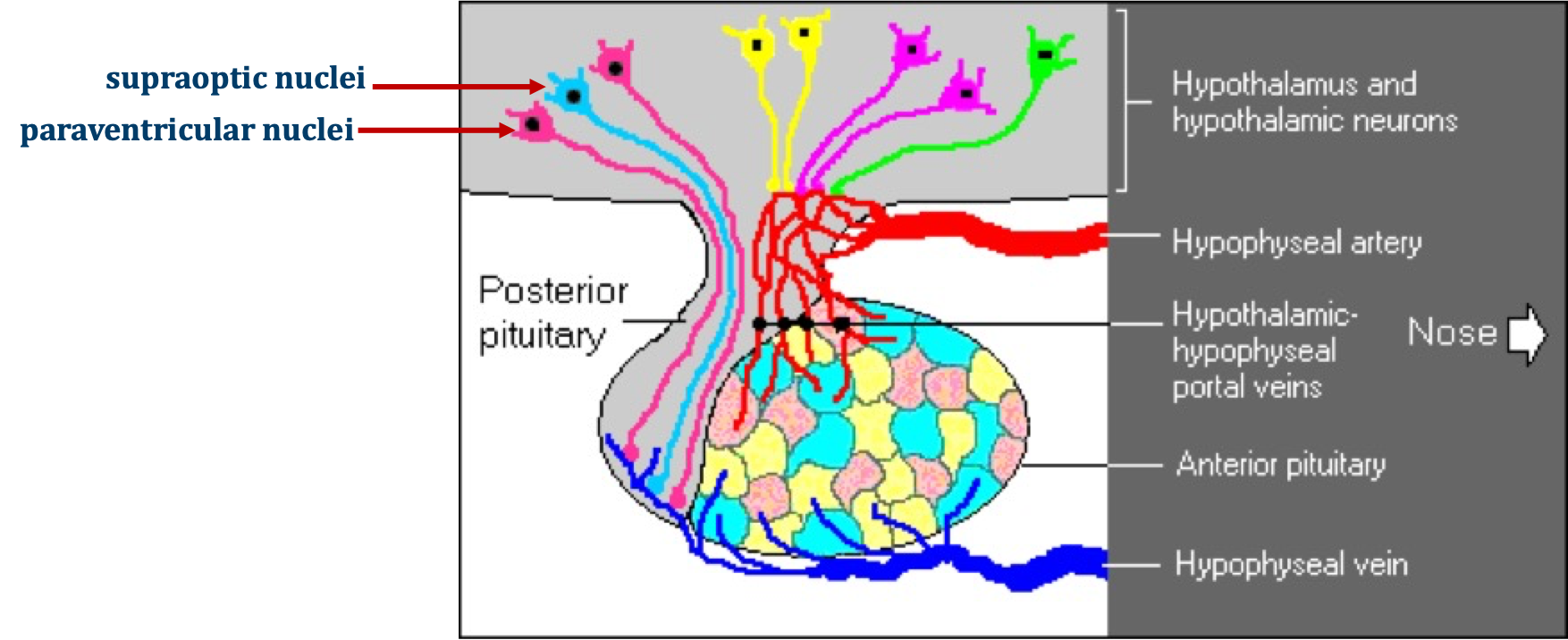
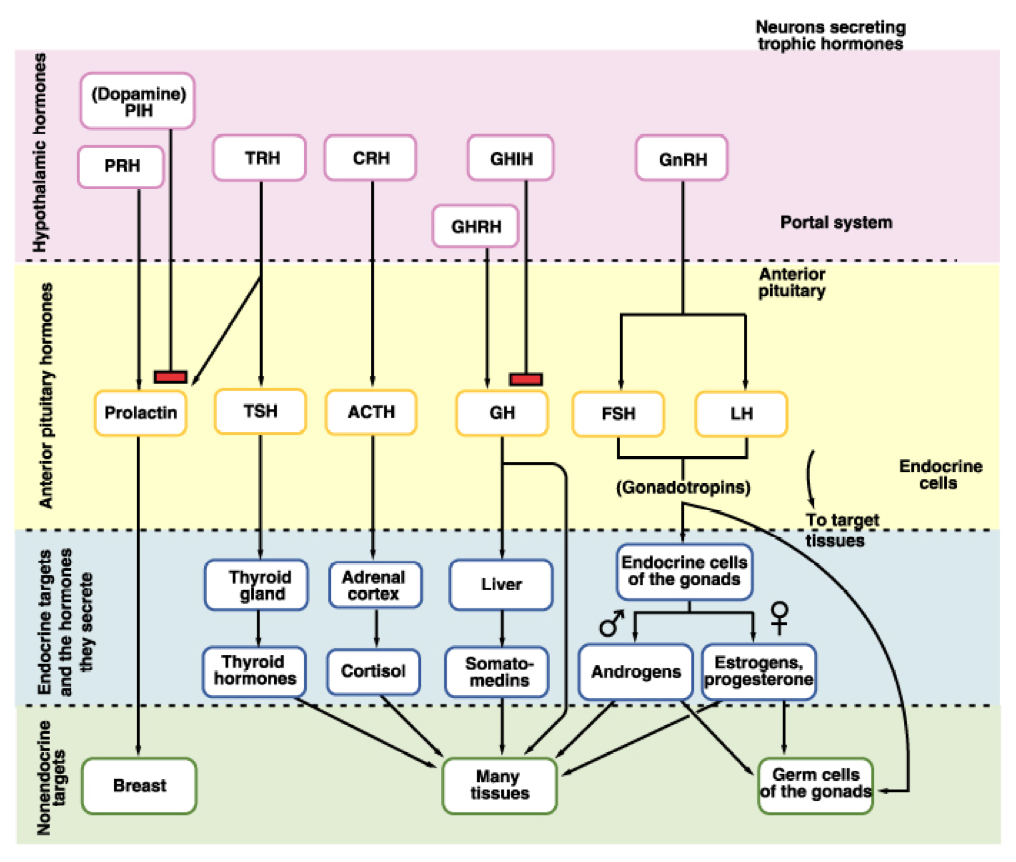
2. Endocrine Control via the Pituitary
- Anterior pituitary: Releasing and inhibiting hormones from the arcuate and paraventricular nuclei regulate hormone secretion (e.g., CRH → ACTH; TRH → TSH; GnRH → LH/FSH).
- Posterior pituitary: ADH and oxytocin produced in the supraoptic and paraventricular nuclei are transported via axons to be released into circulation.
3. Thermoregulation
- Anterior region: Heat loss center (vasodilation, sweating)
- Posterior region: Heat conservation (vasoconstriction, shivering)
4. Regulation of Food and Water Intake
- Lateral zone: Feeding center – stimulation induces eating
- Ventromedial nucleus: Satiety center – stimulation inhibits eating
- Osmoreceptors in the anterior hypothalamus regulate thirst and ADH secretion
5. Circadian Rhythms
- Suprachiasmatic nucleus synchronizes body rhythms (sleep–wake cycles, hormone secretion) with the light–dark cycle
6. Emotional and Behavioral Responses
- Connections with the limbic system influence emotional expression, sexual behavior, and stress responses
7. Memory and Learning
- Mammillary bodies are part of the Papez circuit, essential for memory consolidation
1.3. Clinical Correlations
|
Condition |
Lesion Site |
Effect |
|
Diabetes insipidus |
Supraoptic/paraventricular nuclei or posterior pituitary |
ADH deficiency → excessive urination, thirst |
|
Obesity or anorexia |
Ventromedial or lateral nuclei |
Disturbances in feeding regulation |
|
Sleep disorders |
Suprachiasmatic nucleus |
Disrupted circadian rhythm |
|
Thermoregulatory failure |
Anterior or posterior nuclei |
Inability to regulate body temperature |
|
Memory deficits (e.g., Wernicke–Korsakoff) |
Mammillary bodies |
Anterograde amnesia |
1.4. Introduction to the Pituitary Gland
The pituitary gland (hypophysis) is a small, oval endocrine organ situated at the base of the brain. It serves as the master gland, controlling multiple endocrine glands through its secretion of hormones.
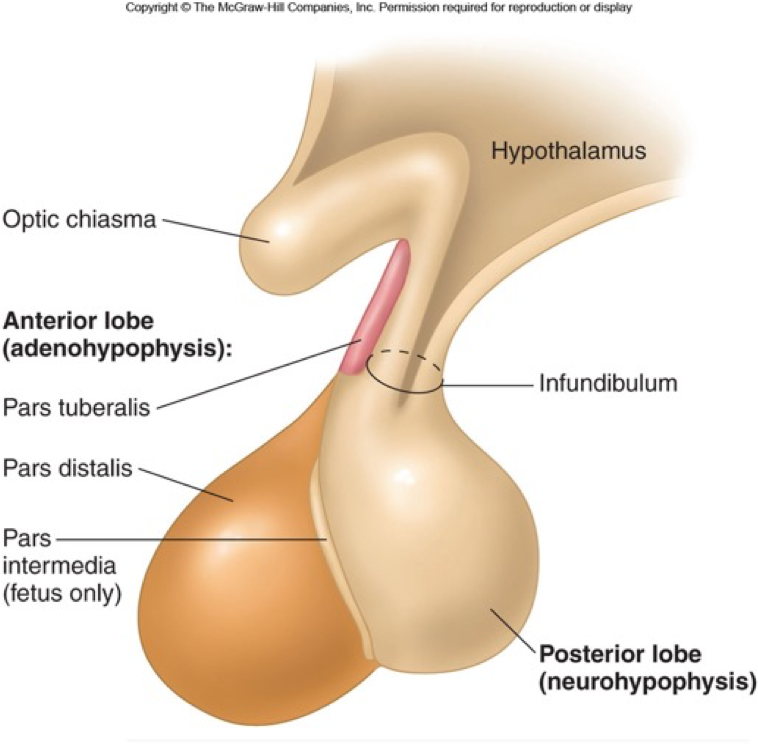
It has two major parts with different embryological origins, anatomical structures, and functions:
- Anterior Pituitary (Adenohypophysis) — glandular in nature, secretes multiple trophic hormones and is controlled by hypothalamic releasing/inhibiting hormones.
- Posterior Pituitary (Neurohypophysis) — neural in origin, stores and releases hypothalamic hormones (ADH, oxytocin).
Location and Relations
- The pituitary gland lies in the sella turcica, a depression in the sphenoid bone at the skull base.
- It is covered superiorly by a fold of dura called the diaphragma sellae, through which the infundibulum (pituitary stalk) passes.
- Superior: Optic chiasm
- Inferior: Sphenoid sinus
- Lateral: Cavernous sinuses (containing internal carotid artery, cranial nerves III, IV, V1, V2, VI)
- Posterior: Dorsum sellae
2. Anterior Pituitary (Adenohypophysis)
Introduction
- The anterior pituitary has no direct neural connection with the hypothalamus.
- Instead, it is regulated by hypothalamic releasing and inhibiting hormones transported through the Hypothalamo–Hypophyseal Portal veins or system (see figure in unit 1.4).
- This unconventional vascular connection between the hypothalamus and posterior pituitary ensures that minute quantities of hypothalamic hormones are carried in a concentrated form directly to their target cells in the anterior pituitary, and are not diluted out in the systemic circulation.
Embryology & Structure
- Derived from Rathke’s pouch, an ectodermal outgrowth of the primitive oral cavity.
- Forms about 75% of the pituitary gland.
- Subdivisions:
- Pars distalis (main secretory portion)
- Pars tuberalis (wraps around infundibulum)
- Pars intermedia (rudimentary in humans)
Hypothalamo–Hypophyseal Portal System
- Hypothalamic neurons release hormones into primary capillary plexus in the median eminence.
- Hormones travel via portal veins to secondary capillary plexus in the anterior pituitary.
- Target secretory cells in the adenohypophysis, stimulating or inhibiting hormone secretion.
Hypothalamic Control of the Anterior Pituitary
The anterior pituitary has no direct neural connection with the hypothalamus. Instead, it is regulated by hypothalamic releasing and inhibiting hormones transported through the hypophyseal portal system (see fig in section 1.4 and below)
- Arcuate nucleus (Tuberal region): major source of releasing/inhibiting hormones
- Paraventricular nucleus: secretes corticotropin-releasing hormone (CRH), thyrotropin-releasing hormone (TRH), and somatostatin
- Preoptic area: secretes gonadotropin-releasing hormone (GnRH)
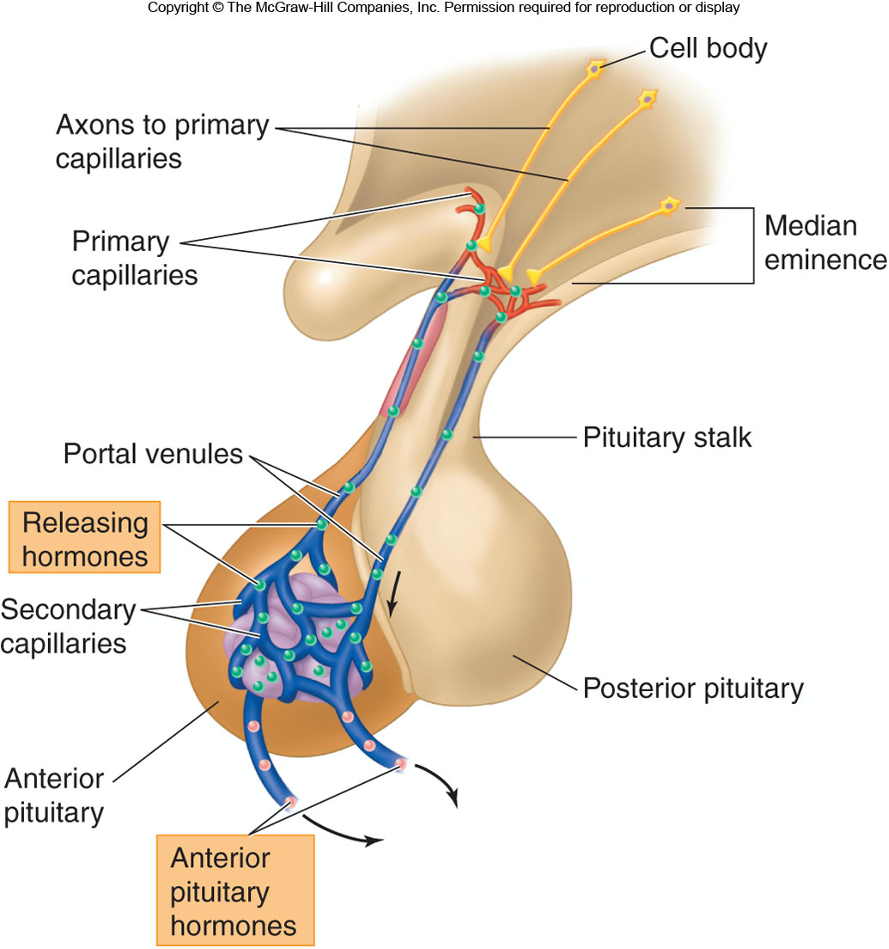
- The anterior pituitary is controlled via releasing and inhibiting hormones produced in the hypothalamus. and
- These hormones are transported to the Anterior Pituitary through the hypothalamo-hypophyseal portal system.
This is the only case in which hormones released into the blood do not go to the entire body
|
Hypothalamic Hormone |
Effect on Anterior Pituitary |
|
Corticotropin-releasing hormone (CRH) |
Stimulate secretion of adrenocorticotropic Hormones (ACTH) |
|
Gonadotropin-releasing hormone (GRH) |
Stimulate secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) |
|
Prolactin-inhibiting hormone (PIH) |
Inhibits prolactin secretion |
|
Somatostatin |
Inhibits secretion of growth hormone |
|
Thyrotropin-releasing hormone (TRH) |
Stimulates secretion of thyroid-stimulating hormone (TSH) |
|
Growth hormone−releasing hormone (GHRH) |
Stimulates growth hormone secretion |
Growth hormone (GH)
Thyroid-stimulating hormone (TSH)
Adrenocorticotropic hormone (ACTH)
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LH)
Prolactin
|
Hormone |
Source Cells |
Target Organ(s) |
Main Function(s) |
|
GH (Growth Hormone) |
Somatotrophs |
Liver, bone, muscle |
Stimulates growth, protein synthesis, IGF-1 secretion |
|
TSH (Thyroid-Stimulating Hormone) |
Thyrotrophs |
Thyroid gland |
Stimulates T₃ and T₄ secretion |
|
ACTH (Adrenocorticotropic Hormone) |
Corticotrophs |
Adrenal cortex |
Stimulates cortisol production |
|
LH (Luteinizing Hormone) |
Gonadotrophs |
Gonads |
Ovulation, corpus luteum, testosterone secretion |
|
FSH (Follicle-Stimulating Hormone) |
Gonadotrophs |
Gonads |
Follicular growth, spermatogenesis |
|
PRL (Prolactin) |
Lactotrophs |
Mammary glands |
Milk production |
|
MSH (Melanocyte-Stimulating Hormone) |
Pars intermedia (rudimentary) |
Skin melanocytes |
Pigmentation (minor role in humans) |
GH → Liver → Growth via IGF
ACTH → Adrenal Cortex → Cortisol release
TSH → Thyroid → Thyroid hormones (T3, T4)
FSH/LH → Gonads → Gametogenesis & sex hormones
PRL → Mammary glands → Milk production and growth of mammary glands
Feedback Control of Anterior Pituitary
Release of tropic hormones is controlled by the hypothalamus which is in turn controlled by the activity of the target glands.
Example: Hypothalamus-Pit-Thyroid Axis
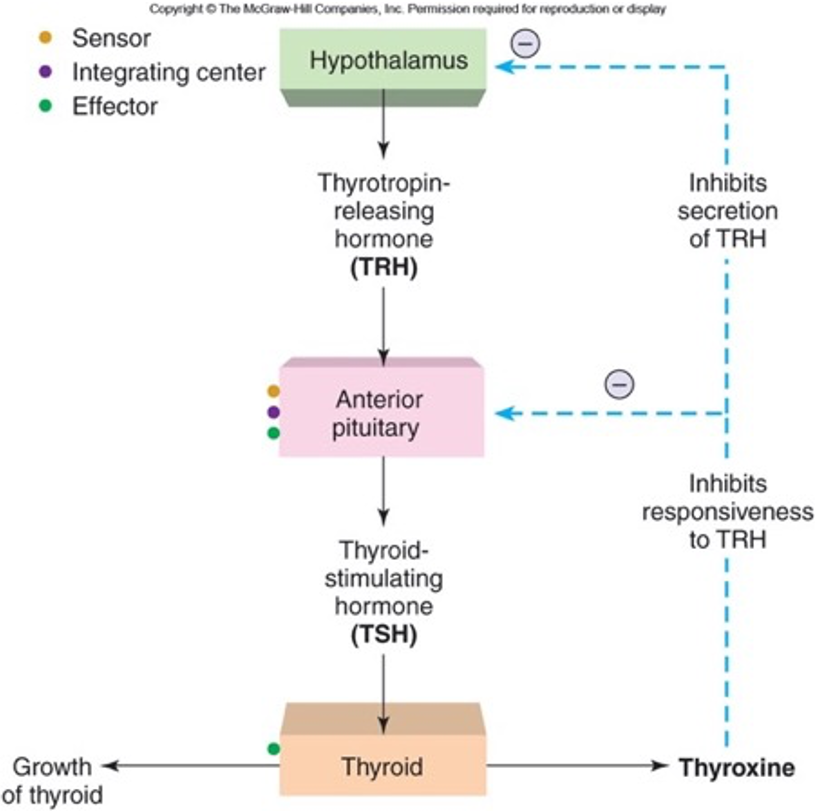
Low levels of thyroxin in the blood stimulate the hypothalamus to secrete thyroid stimulating hormone releasing hormone into the hypophyseal portal system.
The portal system delivers this hormone to the secretory cells of the anterior pituitary which secrete thyroid stimulating hormone (TSH) into general systemic circulation in response.
The blood carries the TSH hormone to the thyroid gland which has cells with receptor proteins for TSH hormone.
Thyroid cells secrete thyroxin into the blood which carries it throughout the body.
Target cells all over the body respond by increasing oxidative RNA synthesis and metabolism.
Cells of the hypothalamus, however, respond to the elevated thyroxin levels by decreasing their production of thyroid stimulating hormone releasing hormone.
This causes the anterior pituitary to decrease production of TSH which in turn causes the thyroid to decrease production of thyroxin.
Blood levels of thyroxin decrease.
The final product regulates secretion of pituitary hormones.
Inhibition can occur at the hypothalamus or pituitary gland level, inhibiting secretion of releasing or stimulating hormones respectively.
Key Points:
- Secretion of anterior pituitary hormones is under hypothalamic regulation except prolactin, which is mainly inhibited by dopamine.
- Blood supply via superior hypophyseal arteries (from internal carotid), forming the portal circulation.
3. Posterior Pituitary (Neurohypophysis)
Embryology & Structure
- Derived from a downward extension of the diencephalon (neuroectoderm).
- Composed mainly of unmyelinated axons and pituicytes (glial-like cells).
- Subdivisions:
- Pars nervosa (main body)
- Infundibular stalk (connects to hypothalamus)
- Median eminence (interface with hypothalamus)
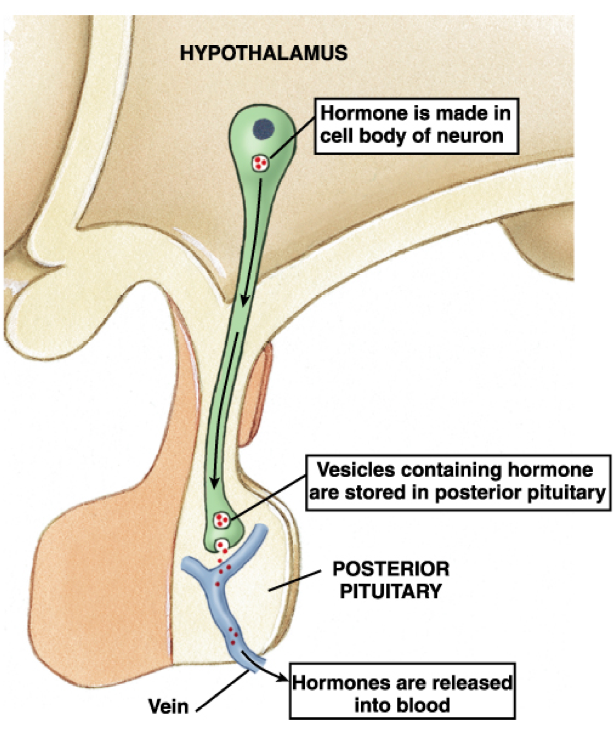
Hypothalamic Nuclei
- Hormones of the posterior pituitary are synthesized in the hypothalamus and transported via the hypothalamo-hypophyseal tract (axonal transport)
|
Hormone |
Site of Synthesis |
Released From |
Main Functions |
|
ADH (Vasopressin) |
Supraoptic nucleus |
Posterior pituitary |
- Increases water reabsorption in collecting ducts (via V₂
receptors) |
|
Oxytocin |
Paraventricular nucleus |
Posterior pituitary |
- Uterine contraction during labor |
- Hormones are synthesized as pre-prohormones, packaged in vesicles, transported down axons, and stored in Herring bodies (axon terminals in posterior pituitary) until release.
Milk Ejection Reflex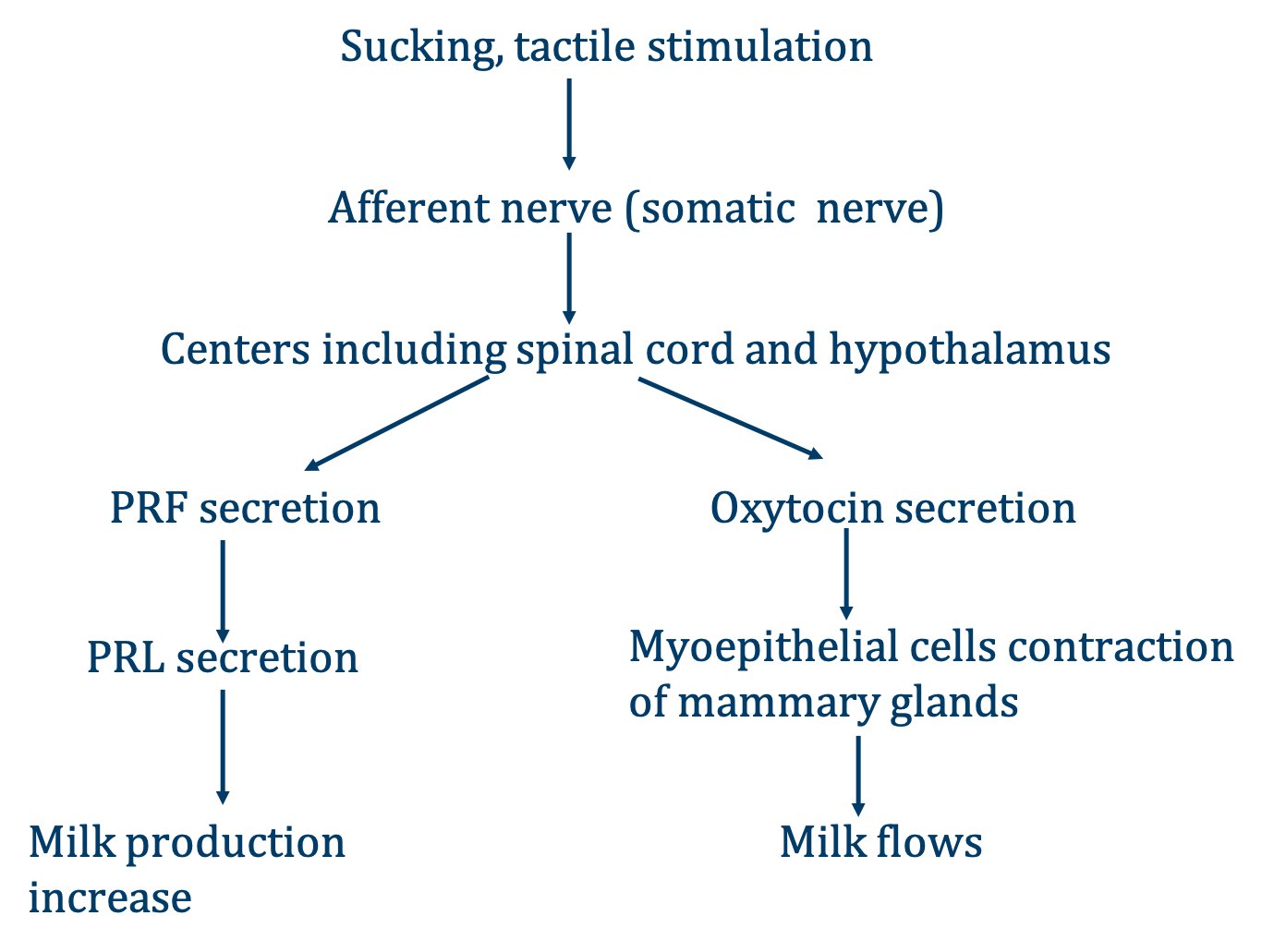
4. Comparative Summary Table
|
Feature |
Anterior Pituitary (Adenohypophysis) |
Posterior Pituitary (Neurohypophysis) |
|
Origin |
Rathke’s pouch (oral ectoderm) |
Neuroectoderm (diencephalon) |
|
Connection to Hypothalamus |
Vascular (portal system) |
Neural (hypothalamo-hypophyseal tract) |
|
Main Nuclei |
Arcuate, Paraventricular (releasing hormones), Preoptic |
Supraoptic, Paraventricular (hormone synthesis) |
|
Type of Tissue |
Glandular |
Neural |
|
Main Hormones |
GH, TSH, ACTH, LH, FSH, PRL, MSH |
ADH, Oxytocin |
|
Mode of Hormone Transport |
Hypothalamic hormones via portal blood |
Hormones synthesized in hypothalamus, transported along axons |
|
Blood Supply |
Superior hypophyseal arteries → portal system |
Inferior hypophyseal arteries |
|
Main Function |
Secretes trophic hormones controlling peripheral endocrine glands |
Stores and releases hypothalamic hormones |
5. Regulatory Pathways – Hormonal Control of Growth, Metabolism, and Reproduction
- Hypothalamic-pituitary-thyroid axis: TRH → TSH → T3/T4 → metabolism.
- Hypothalamic-pituitary-adrenal axis: CRH → ACTH → cortisol → stress response.
- Hypothalamic-pituitary-gonadal axis: GnRH → LH/FSH → estrogen/testosterone → reproduction
6. Clinical Correlations
|
Condition |
Site Involved |
Effect |
|
Pituitary adenomas |
Anterior pituitary |
Hormone hypersecretion (e.g., prolactinoma → galactorrhea, infertility) or mass effects |
|
Hypopituitarism |
Anterior pituitary |
Deficiency of one or more hormones → growth failure, hypothyroidism, adrenal insufficiency |
|
Diabetes insipidus |
Posterior pituitary or supraoptic nucleus |
ADH deficiency → polyuria, polydipsia |
|
Syndrome of Inappropriate ADH Secretion (SIADH) |
Posterior pituitary (ADH excess) |
Water retention, hyponatremia |
|
Sheehan’s syndrome |
Anterior pituitary (postpartum necrosis) |
Failure to lactate, amenorrhea, secondary hypothyroidism/adrenal insufficiency |
- Hypersecretion of GH leads to cause gigantism in children and acromegaly in adult.
- Hyposecretion of GH results in dwarfism during childhood.
7. Key Points Summary
- The anterior pituitary is glandular, controlled by hypothalamic releasing/inhibiting hormones via the portal system, and secretes trophic hormones.
- The posterior pituitary is neural, acts as a storage and release site for hypothalamic hormones ADH and oxytocin.
- Hypothalamic
nuclei:
- Arcuate & paraventricular (releasing hormones) → anterior pituitary regulation
- Supraoptic & paraventricular (ADH/oxytocin) → posterior pituitary outpu
- Disorders can involve hypersecretion, hyposecretion, or mass effects