Lecture Notes: Sexual Differentiation, Sex Determination, and Gametogenesis
| Site: | Newgate University Minna - Elearning Platform |
| Course: | Endocrine and Reproductive System |
| Book: | Lecture Notes: Sexual Differentiation, Sex Determination, and Gametogenesis |
| Printed by: | Guest user |
| Date: | Friday, 9 January 2026, 8:35 PM |
1. Introduction
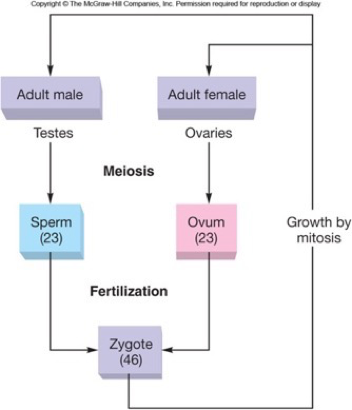
· Sexual reproduction is the process by which two specialized reproductive cells—gametes (sperm and ovum)—fuse to form a zygote, leading to the formation of a new individual.
· It promotes genetic variation, ensuring diversity and adaptability of the human species.
· Sexual development in humans progresses through:
o Chromosomal Sex Determination
o Gonadal Differentiation
o Phenotypic Sexual Differentiation
· Gametogenesis (spermatogenesis and oogenesis) forms the functional male and female gametes.
Learning Objectives
· Explain mechanisms of chromosomal sex determination.
· Describe gonadal development and sexual differentiation pathways.
· Discuss hormonal influences on internal and external genitalia development.
· Outline the steps of spermatogenesis and oogenesis.
2. Sex Determination
- Sex determination is the process by which an organism's biological sex is established, primarily through genetics or environmental factors.
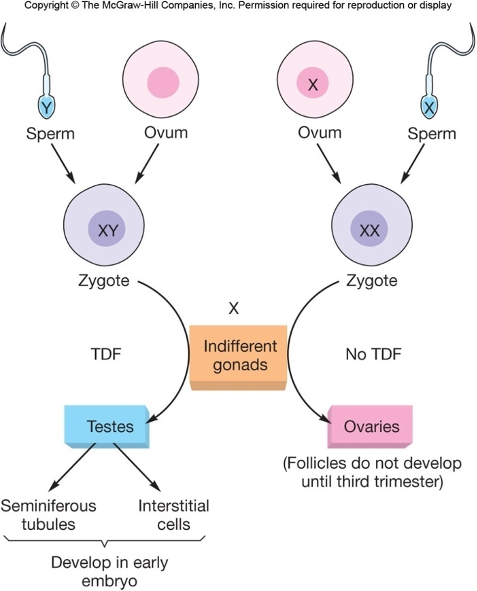
- In humans, it's genetic, where the inheritance of an X and Y chromosome (XY) typically results in a male, and two X chromosomes (XX) results in a female.
- To understand how the determination of sex happens, we need to know the following process.
- Humans have 23 pairs of chromosomes. Out of these 23 pairs, 22 pairs are Autosomes and only one pair is the ‘Sex Chromosome’, which actively takes part in the process of sex determination.
- Both males and females carry two sets of sex chromosome.
- Male has one X and one Y (XY) sex chromosome in which both are active
- Female has both X (XX) sex chromosome in which one is active.
- The XY sex-determination system is found in humans, mammals, in some insects, and in few plant species.
- All children will inherit an X chromosome from their mother, despite whether they are a boy or girl. Thus, the sex of the children will be determined by the type of chromosome inherited from their father.
- A child who inherits Y chromosome will be a boy and who inherits X chromosome will be a girl.
2.1. Genetic (Chromosomal) Sex
· Determined at fertilization when the embryo receives either:
o 46,XX → Genetic Female
o 46,XY → Genetic Male
· This initial event determines whether the gonads will develop as testes or ovaries
· The presence or absence of the Y chromosome is pivotal.
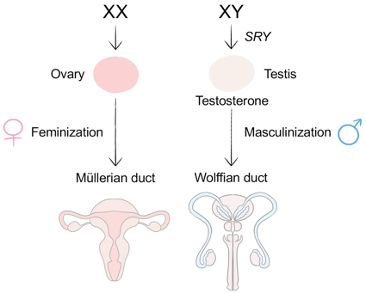
2.2. SRY Gene (Sex-determining Region of Y)
· Located on the short arm of the Y chromosome.
· Encodes Testis Determining Factor (TDF).
· Initiates bipotential gonad differentiation into testes.
· Absent in XX embryos → ovarian pathway proceeds by default.
2.3. Gonadal Development
· Gonads arise from intermediate mesoderm and genital ridges (week 4–6).
· If SRY/TDF present → Sertoli cells differentiate by week 6–7.
· If SRY absent → ovaries develop starting weeks 8–9.
2.4. Disruptions in Sex Determination
- Turner syndrome (45, X0)
- Streak ovaries, short stature, infertility.
- Klinefelter syndrome (47, XXY)
- Testicular atrophy, gynecomastia, infertility.
- Androgen insensitivity syndrome (XY)
- Testes present but external genitalia develop as female due to androgen receptor defect.
3. Sexual Differentiation
3.1 Overview
· Sex differentiation: the process by which a developing embryo or fetus develops into a male or female sexual phenotype.
· It's a complex process involving genetic, hormonal, and anatomical changes that lead to the development of distinct male and female characteristics
- Early embryo has indifferent gonads capable of developing into either testes or ovaries.
- The gonadal ridge can develop into either testes or ovaries.
- Supporting structures include the mesonephric (Wolffian) and paramesonephric (Müllerian) ducts
- Presence or absence of SRY gene and testicular hormones determines the direction of development.
- Key Stages of Sexual Differentiation
- Chromosomal sex (XX or XY)
- Gonadal sex (ovaries or testes)
- Phenotypic sex (internal & external genitalia)
- Secondary sexual characteristics
3.2 Differentiation of Internal Genitalia (Gonadal sex)
· Development depends on presence or absence of testes and their hormones.
· Male Differentiation
o Triggered by SRY gene → TDF → Sertoli cell development.
o Sertoli cells secrete Anti-Müllerian Hormone (AMH) → regression of Müllerian ducts.
o Leydig cells produce testosterone, promoting the development of:
§ Wolffian ducts → epididymis, vas deferens, seminal vesicle.
§ Dihydrotestosterone (DHT) forms external genitalia (penis, scrotum, prostate).
· Female Pathway (No Testes)
o In absence of SRY and AMH → Müllerian ducts form:
§ Fallopian tubes
§ Uterus
§ Upper vagina
o No testosterone → Wolffian ducts regress.
· Role of the SRY Gene
o Located on the Y chromosome.
o Codes for Testis-Determining Factor (TDF).
o Initiates differentiation of Sertoli cells → triggers testis formation.
o Absence of SRY allows ovarian development to occur by default
3.3 Differentiation of External Genitalia (Phenotypic sex)
· Driven by androgen exposure from weeks 8–12.
· Male
o DHT (from testosterone) causes formation of:
§ Penis
§ Scrotum
§ Prostate
· Female
o In absence of DHT:
§ Clitoris
§ Labia majora/minora
§ Lower vagina
3.4 Regulation of Sexual Differentiation
Regulation in Males
· Sertoli Cells
o Produce Anti-Müllerian Hormone (AMH)
o Causes regression of Müllerian ducts, preventing female internal organ formation.
· Leydig Cells
o Produce testosterone
o Testosterone converts Wolffian ducts into:
§ Epididymis
§ Vas deferens
§ Seminal vesicles
o Testosterone is converted by 5α-reductase to Dihydrotestosterone (DHT)
· DHT and External Genitalia
o DHT is responsible for:
§ Development of penis
§ Formation of scrotum
§ Growth of the prostate
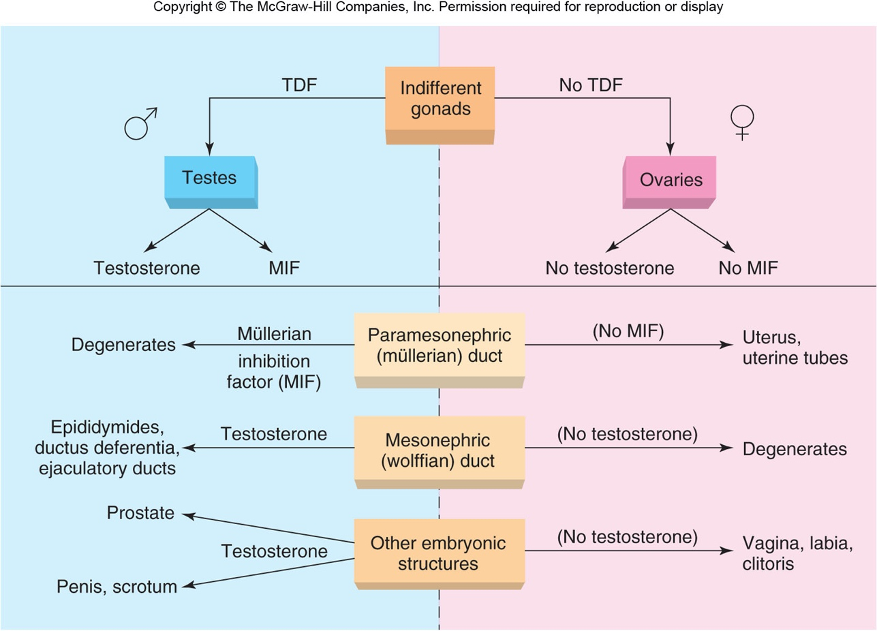
Regulation in Females
· Absence of SRY
o Gonad → ovary.
· Absence of AMH
o Müllerian ducts develop into:
§ Fallopian tubes
§ Uterus
§ Upper vagina
· Absence of Testosterone
o Wolffian ducts regress.
· In the absence of DHT, the external phenotype becomes:
o Clitoris
o Labia majora/minora
o Lower vagina
4. Disorders of Sexual Differentiation (DSDs)
· 5α-reductase deficiency.
- Inability to convert testosterone to DHT
- Ambiguous genitalia at birth; masculinization at puberty
· Androgen insensitivity syndrome (AIS) ) or Male pseudo hermaphroditism
o XY individual with non-functional androgen receptors → female external phenotype without uterus or fallopian tubes
· Congenital adrenal hyperplasia (CAH) or Female pseudo hermaphroditism
o XX individual with excess androgen production by the adrenal gland → virilized external genitalia.
· Hermaphroditism or Ovotesticular DSD
o a rare condition in which an individual possesses both ovarian and testicular tissue—either in the same gonad (ovotestis) or in opposite gonads.
§ 46,XX testicular DSD: Translocation of SRY to X chromosome.
§ 46,XY gonadal dysgenesis: Mutations in SRY or downstream genes.
Causes of DSDs
1. Genetic Factors:
◦ Many DSDs have a genetic basis, involving mutations in genes responsible for sex determination and development.
2. Hormonal Factors:
◦ Imbalances or deficiencies in hormones like androgens or other sex hormones can lead to DSDs.
3. Environmental Factors:
◦ While less understood, environmental factors may also play a role in some cases.
5. Gametogenesis
5.1 Definition
· Gametogenesis is the biological process by which haploid gametes (sperm and ova) are formed from diploid germ cells through meiotic cell division and cellular differentiation.
o In males, this process is called spermatogenesis.
o In females, it is called oogenesis.
· Begins in fetal life for females; at puberty for males.
· The ultimate goal of gametogenesis is to produce mature, functional gametes capable of fertilization, restoring the diploid chromosome number in the resulting zygote.
5.2 Origin of Germ Cells
§ Primordial germ cells (PGCs) originate in the yolk sac endoderm during early embryonic development.
§ They migrate to the developing gonadal ridge (future testes or ovaries) by the 6th week of gestation.
§ Once in the gonads, these cells multiply by mitosis and later enter meiosis to form gametes.
5.3 Common Features
- Both involve meiosis → haploid gametes.
- Begin from primordial germ cells (PGCs).
- Require support from surrounding somatic cells:
- Sertoli cells in testes
- Granulosa cells in ovary
5.1. Spermatogenesis
5.1 Location and Timeline
- Occurs within seminiferous tubules of testes.
- Supported by Sertoli cells (“nurse cells”).
- Entire cycle takes ~74 days.
- Continuous from puberty throughout life.
5.2 Phases of Spermatogenesis
- Spermatocytogenesis:
a. Mitotic proliferation of spermatogonia (diploid stem cells) → primary spermatocytes.
§ Type A → stem cells
§ Type B → commit to meiosis
b. Meiosis I: primary spermatocytes → secondary spermatocytes.
c. Meiosis II: secondary spermatocytes → spermatids.
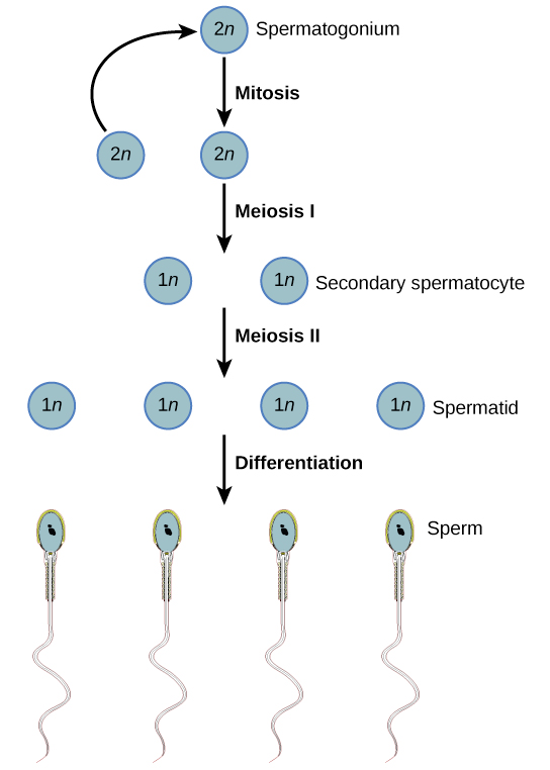
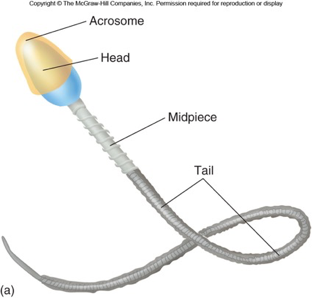
2. Spermiogenesis:
a. Spermatids transform into mature spermatozoa
b. Formation of acrosome, flagellum, nuclear condensation.
3. Spermiation
-
- Release of mature sperm into lumen.
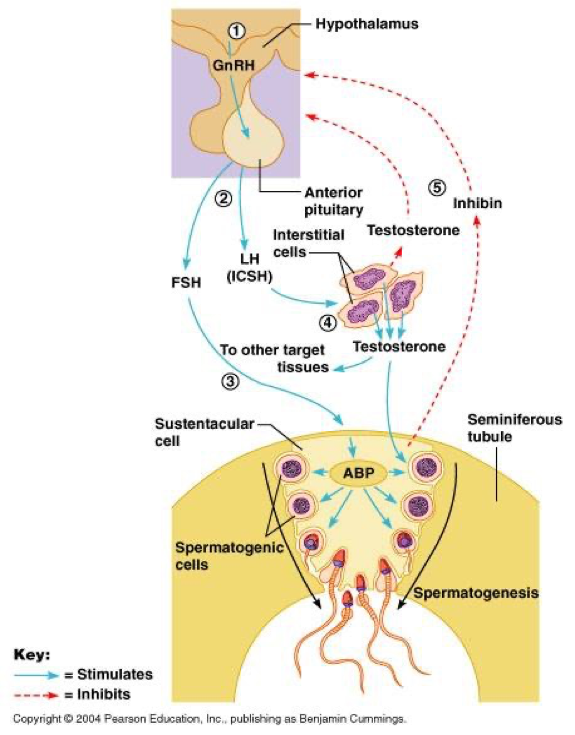
5.3 Hormonal Regulation
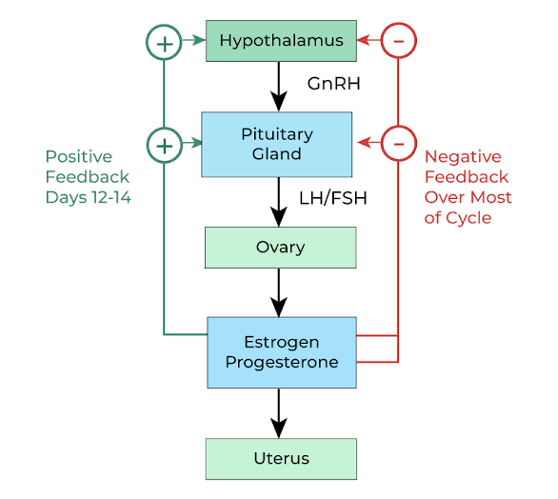
- GnRH (from hypothalamus) → stimulates anterior pituitary to release:
- FSH → stimulates Sertoli cells
- LH → stimulates Leydig cells to produce testosterone
- Testosterone + FSH → essential for completion of spermatogenesis
- Inhibin B from Sertoli cells → negative feedback to pituitary
5.2. Oogenesis
6.1 Location
· ogenesis is the process by which female gametes (ova or eggs) develop from oogonia (germ cells) within the ovaries.
· Occurs in ovaries within ovarian follicles.
· It involves multiplication, growth, and maturation, resulting in the formation of a single functional ovum capable of being fertilized.
6.2 Stages of Oocyte Development
Unlike spermatogenesis, oogenesis begins before birth (oogonia → primary oocytes), pauses for many years, and resumes at puberty, continuing cyclically until menopause.
- Fetal (Pre-natal) Phase
- The primordial germ cells (PGCs) migrate into the developing ovaries and differentiate into oogonia (immature egg cells)
- Oogonia (diploid) proliferate (until 5th month of gestation by mitosis → to produce 6 to 7 million germ cells
- These germ cells develop into primary oocytes (most most of these degenerates before birth - atresia)
- Primary oocytes begin Meiosis I but are arrested in prophase I until puberty.
- This arrested state may last 10–50 years, depending on when ovulation occurs.
- At birth, about 1–2 million primary oocytes are present; by puberty, only about 300,000–400,000 remain.
- Puberty to menopause
- Monthly cohorts resume meiosis
- One primary oocyte completes Meiosis I → forms a secondary oocyte and a small polar body.
- The polar body allows for the oocyte to get rid of chromosomes while at the same time taking the least amount of resources (cytoplasm) from the oocyte
- The secondary oocyte begins Meiosis II but arrests at metaphase II until fertilization.
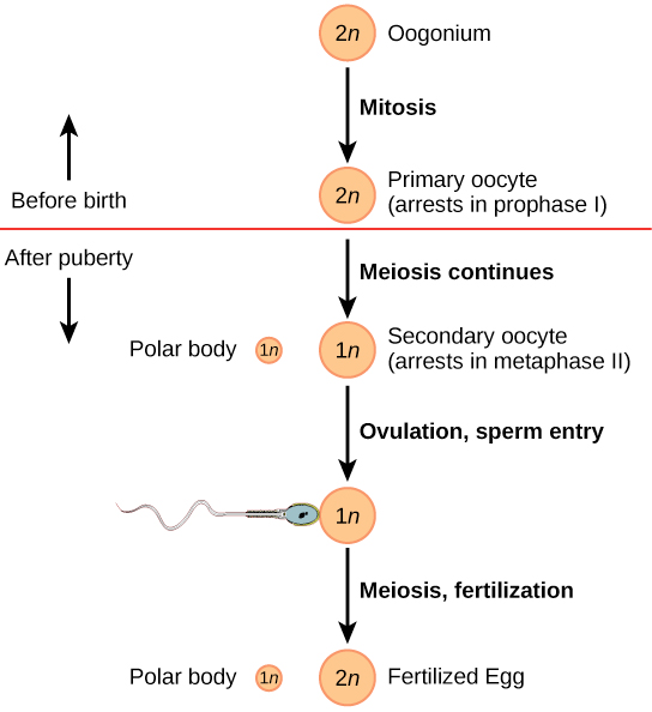
3. Ovulation
o Secondary oocyte arrests in meiosis II.
4. Fertilization
-
- Completion of meiosis II only if fertilized.
6.3 Folliculogenesis
· Primordial follicle
· Primary follicle
· Secondary follicle
· Graafian follicle
· Corpus luteum formation post-ovulation
6.4 Hormonal Regulation
-
- FSH
- Stimulates follicular growth
- LH
- Triggers ovulation
- Supports corpus luteum formation
- Estrogen and progesterone
- Regulate endometrium
- Provide feedback to hypothalamus/pituitary
- FSH
5.3. Clinical Correlations
· Infertility: low sperm count, anovulation, PCOS.
· Hormonal disorders: hypogonadism, hyperprolactinemia.
· Reproductive toxicology: radiation, chemotherapy effects on gametes.
6. Summary
- · Sex determination depends on chromosomes and SRY gene.
- Sexual differentiation proceeds through chromosomal → gonadal → phenotypic stages.
- SRY gene and testicular hormones drive male development.
- Gametogenesis involves mitosis, meiosis, and maturation of sperm and oocytes.
- Disorders of sexual differentiation arise from genetic or hormonal abnormalities.
7. Self-Assessment Questions
- Outline the three major stages of sexual differentiation.
- What is the role of AMH in male development?
- Describe the main phases of spermatogenesis.
- At what stage does the oocyte arrest during fetal life?
- Explain how DHT contributes to male genital development.