Lecture Notes on Male and Female Reproductive Physiology
| Site: | Newgate University Minna - Elearning Platform |
| Course: | Endocrine and Reproductive System |
| Book: | Lecture Notes on Male and Female Reproductive Physiology |
| Printed by: | Guest user |
| Date: | Friday, 9 January 2026, 8:23 PM |
1. Overview of the Reproductive System
1.1 Introduction
- The reproductive system ensures the continuation of the human species.
- Involves reproductive organs, endocrine glands, gamete formation, and hormonal cycles.
- Male system focuses on sperm production and delivery.
- Female system focuses on oocyte maturation, fertilization, and support of pregnancy.
1.2 Key Functions
- Gametogenesis (spermatogenesis & oogenesis)
- Sex hormone production (testosterone, estrogen, progesterone)
- Reproductive behaviour
- Support of embryonic and fetal development (female)
2. Male Reproductive Anatomy
2.1 External Genitalia
- Penis: urethra, glans, erectile tissue (corpora cavernosa & corpus spongiosum).
- Scrotum: houses testes; temperature regulation (≈34°C).
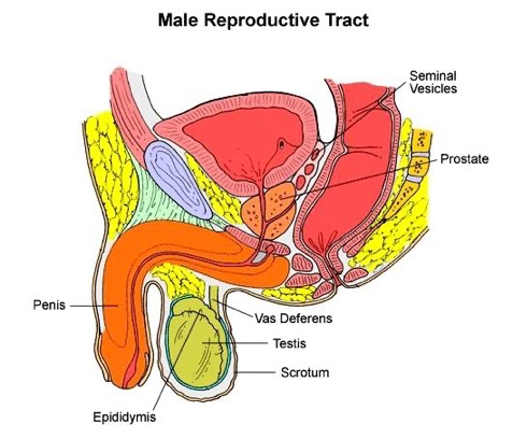
2.2 Internal Reproductive Structures
- Testes: seminiferous tubules (sperm production), Leydig cells (testosterone).
- Epididymis: sperm maturation & storage.
- Vas deferens: transport of sperm.
- Accessory glands:
- Seminal vesicles (60% semen volume)
- Prostate gland (enzymes, citrate)
- Bulbourethral glands (lubrication)
2.3 Blood-Testis Barrier
- Formed by tight junctions of Sertoli cells.
- Protects germ cells from immune system.
- Maintains specialized microenvironment for spermatogenesis.
2.4: Male Sexual Response
- The main phases of the male sexual response are:
- erection
- emission and
- ejaculation.
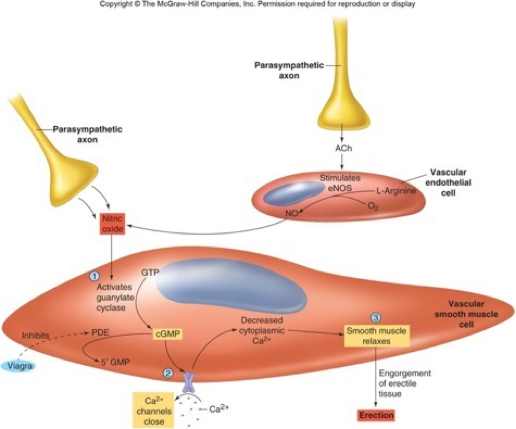
2.4.1 Erection
- Erection results from engorgement of the erectile bodies with blood.
- Can occur due to conscious sexual thought
- hypothalamus sacral region of the spinal cord penis), or
- sensory stimulation: penis spinal cord penis
- Parasympathetic (S2–S4) → nitric oxide release → vasodilation → erection.
- Activation of parasympathetic nerves to the penis increases local nitric oxide (NO) release
- NO results in increased blood flow into and engorgement of the erectile tissues of the penis.
- This results in an erection, which allows the penis to penetrate the vagina.
- Inhibited by stress, sympathetic activity.
2.4.2 Emission and Ejaculation
- Emission is the movement of semen into the urethra
- Ejaculation is the forceful expulsion of semen from the urethra due to rhythmic contraction of pelvic muscles.
- Both are under sympathetic nervous system control.
- Contraction of smooth muscles in the tubules, seminal vesicle, prostate, and muscles at base of penis is involved in ejaculation.
- Detumescence
- erection subsides: sympathetic constricts arterioles
- latent period: new ejaculation not possible (min-hrs)
2.5 Semen
§ Semen, also known as seminal fluid or ejaculate, is the whitish-gray fluid released by males during sexual climax (ejaculation).
§ These fluids originate from the testicles, seminal vesicles, and prostate gland.
§ Function:
o Semen's primary role is to carry sperm to the female reproductive tract for fertilization.
o It also provides a nutrient-rich environment for sperm survival and motility.
§ 2-5ml/ejaculation contains;
o 60% seminal fluid from seminal vesicles (fructose, amino acids, citric acid, phosphorus, potassium, and prostaglandins)
o 30% prostatic fluid from the prostate gland (citric acid, acid phosphatase, calcium, sodium, zinc, potassium, enzymes, and fibrolysin);
o 10% testicular fluid from testes (50-300million sperm/ml; less than 60 million total = sterile).
§ Characteristics
o Appearance: Typically grey-opalescent, it initially clots and then liquefies over time.
o Volume: The average volume is about 1 to 5 milliliters per ejaculate.
o Smell/Taste: It can have a chlorine-like or slightly fishy odor and a slightly sweet taste due to fructose.
o pH: It is slightly alkaline, with a pH range of 7.2 to 7.8, which helps protect sperm in the acidic environment of the vagina.
§ Everyday a healthy adult male produce about 400 million sperm.
2.6 Clinical Note
- Fertility and sexual function decline with age due to declining levels of sex hormones
- age 50 men go through a period of physical and psychological change = climacteric
- older men are also more likely to father children with autism, epilepsy or schizophrenia
- A sperm count < 20 million/ml semen is called oligospermia and is considered less fertile. May be caused by heat, drugs, or anabolic steroids
- Erectile dysfunction: vascular, neurogenic, endocrine, or psychogenic causes.
3. Female Reproductive Anatomy
3.1 External Genitalia
- Vulva, labia majora, labia minora, clitoris (homologous to male penis), vestibule.
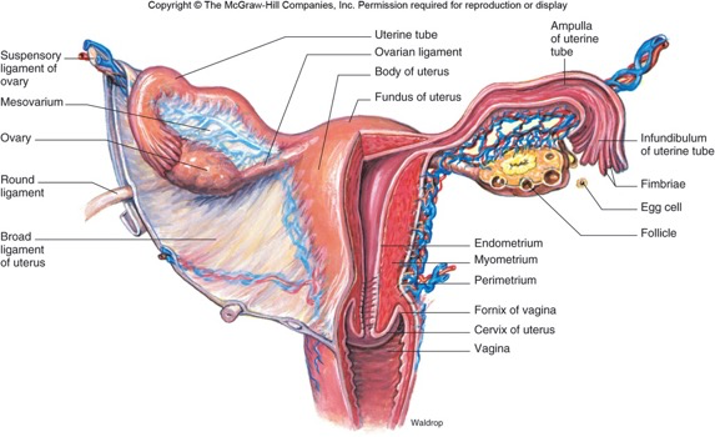
2.2 Internal Structures
- Ovaries: oogenesis & hormone production (estrogens, progesterone and inhibin).
- Fallopian tubes: fertilization site.
- Uterus: implantation and fetal development.
- Cervix: mucus plug, sperm transport.
- Vagina: birth canal, sexual intercourse.
2.3 Ovarian Follicles
- Primordial → primary → secondary → antral → Graafian follicles.
- Each contains an oocyte + granulosa + theca cells.
2.4 Female Sexual Response
Arousal
- Parasympathetic → increased blood flow → clitoral erection, lubrication.
Orgasm
- Rhythmic contractions of pelvic muscles.
- No refractory period (unlike males).
2.5 Clinical Note
- Sexual dysfunction may be hormonal, psychological, neurological, or vascular.
4. Ovarian and Menstrual cycles
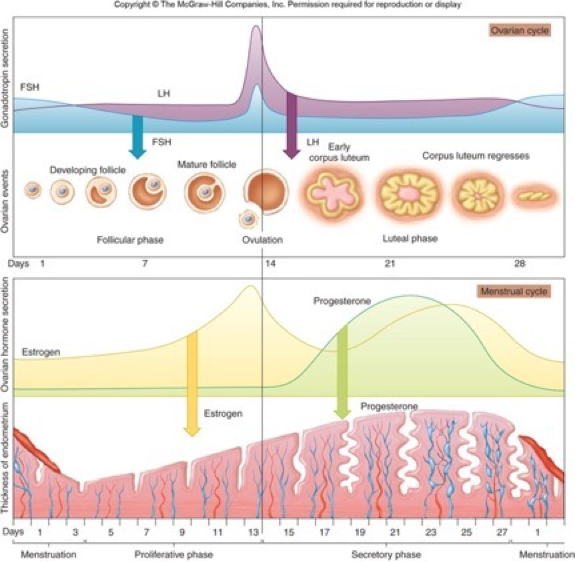
- The ovarian and menstrual cycles are two coordinated monthly processes in the female reproductive system, where the ovarian cycle develops an egg in the ovary (follicular phase, ovulation, luteal phase), and the uterine (menstrual) cycle prepares the uterus lining (proliferative, secretory, menstrual phases) for potential pregnancy, all regulated by hormones like FSH, LH, estrogen, and progesterone, typically around 28 days.
- These cycles run in parallel: the ovarian follicular phase aligns with the uterine proliferative phase, and the ovarian luteal phase with the uterine secretory phase, ending in menstruation if no pregnancy occurs
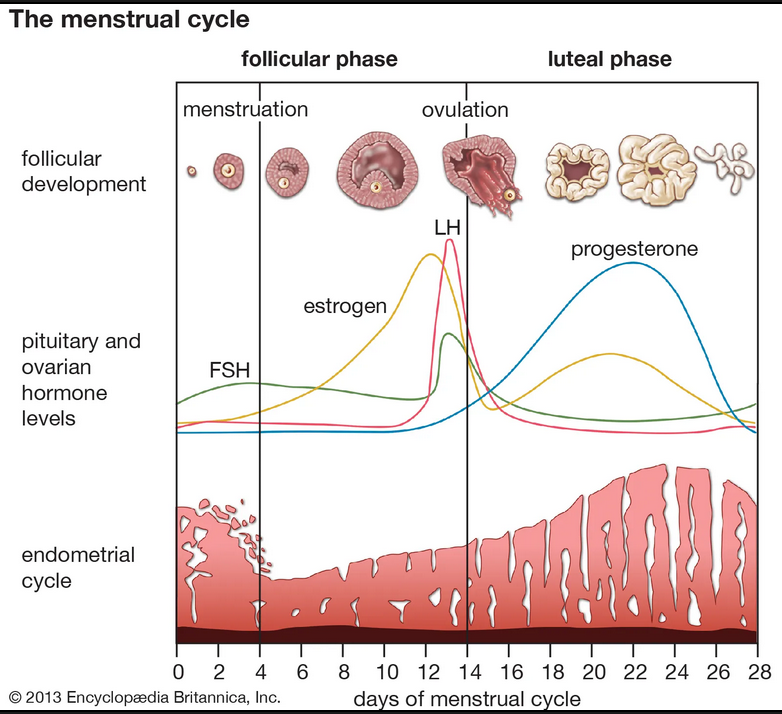
Ovarian Cycle Phases (Ovary)
- Follicular Phase: FSH & LH stimulate follicles to grow, producing estrogen. One becomes dominant.
- Ovulation: A surge in LH causes the dominant follicle to rupture, releasing the egg (around day 14).
- Luteal Phase: The ruptured follicle becomes the corpus luteum, producing progesterone and estrogen to ready the uterus. If no pregnancy, it degenerates.
- Menstrual Phase: Low hormone levels cause the uterine lining (endometrium) to shed (period).
- Proliferative Phase: Rising estrogen rebuilds the endometrium.
- Secretory Phase: Progesterone (from corpus luteum) makes the lining rich in glands and blood vessels, ready for implantation.
- FSH (Follicle-Stimulating Hormone): Stimulates follicle growth.
- LH (Luteinizing Hormone): Triggers ovulation (LH surge).
- Estrogen: Thickens the uterine lining; high levels trigger LH surge.
- Progesterone: Maintains the uterine lining for pregnancy.
- Beginning: Day 1 of menstruation marks the start of both cycles.
- Correlation: Ovarian follicular phase = Menstrual & Proliferative phases; Ovarian luteal phase = Secretory phase.
- End: Hormone drop (estrogen/progesterone) causes the corpus luteum to degenerate, leading to menstruation and a new cycle
4.1. Ovarian Cycle (28-Day Cycle)
1.1 Overview
§ The monthly series of events associated with egg maturation is the ovarian cycle.
§ It consists of three phases.
1. The follicular phase
2. Ovulation phase.
3. Luteal Phase
§ Regulated by the hypothalamic–pituitary–ovarian (HPO) axis.
§ Ovarian cycles may vary in length. Average length: 28 days (normal range: 21–35 days).
o The follicular phase may range from seven to 26 days long. However, the luteal phase is constant 14 days.
1.2 Follicular Phase (Day 1–14)
- Begins with menstruation.
- Rising FSH stimulates a cohort of primordial follicles to develop into primary follicles.
- Continued follicular growth results in fused vesicles to form a single antrum. This is a mature Graafian follicle
- As the Graafian follicle grows, the primary oocyte finishes meiosis I to become a secondary oocyte (plus a polar body, which soon degenerates).
- Dominant follicle selected by Day 7.
- Granulosa cells produce estrogen.
- Endometrial proliferation
- Cervical mucus thinning
- Estrogen peak → LH surge (positive feedback)→ ovulation.
- The follicles that did not rupture degenerate and their eggs are lost.
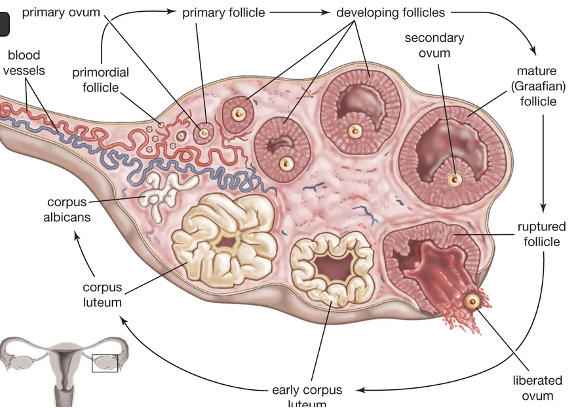
1.3 Ovulation (Around Day 14)
- The spike in LH causes ovulation: the most mature follicle bulges out of the ovary, ruptures and releases its egg (secondary oocyte arrested in metaphase II).
- LH surge begins ~24 hours before ovulation.
- Stimulates Graafian follicle to rupture, releasing secondary oocyte
- Fertilization must occur within 12–24 hours.
- If not fertilized, the oocyte will degenerate after a few days.
1.4 Luteal Phase (Day 15–28)
- Ruptured follicle → corpus luteum under the influence of LH
- Secretes progesterone (dominant) + estrogen.
- The progesterone facilitates the regrowth of the uterine lining and inhibits the release of further FSH and LH.
- The inhibition of FSH and LH prevents any further eggs and follicles from developing, while the progesterone is elevated.
- If no pregnancy: corpus luteum degenerates → corpus albicans →hormonal level falls → menstruation begins.
- The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles again.
- If the oocyte is fertilized and pregnancy occurs, the corpus luteum will persist for about three months until the placenta is formed and ready to take over its function
4.2. Uterine (Endometrial) Cycle
1.1 Overview
§ The menstrual cycle describes the 28-day cycle of endometrial buildup and sloughing in response to ovarian hormones.
§ Three phases:
1. Proliferative: proliferation of endometrium and increase in blood vessels (spiral arteries)
2. Secretory: development of endometrium — thick, vascular, spongy — in preparation for the embryo
3. Menstrual: constriction of spiral arteries cell death and sloughing of layer of endometrium. Bleeding phase
§ Changes in the endometrium follow changes in the follicles of the ovaries.
1.2 Menstrual Phase (Day 1–5).
- Shedding of functional layer of endometrium.
- Occurs as a result of the fall in estrogen and progesterone when the corpus luteum degenerates
- Arteries in the endometrium constrict, cells in the stratum functionale die, and this region is sloughed.
1.3 Proliferative Phase (Day 6–14)
- Estrogen → endometrial thickening, cell proliferation.
- Occurs while ovary is in the follicular phase
- Increasing levels of estrogen stimulate the growth (cell proliferation ) of the stratum functionale of the endometrium leading to endometrial thickening.
- The endometrium also becomes more vascular and develops LH receptors.
1.4 Secretory Phase (Day 15–28)
- Occurs while the ovaries are in the luteal phase
- Secretion of progesterone stimulates the development of uterine glands, which store glycogen.
- Progesterone → glandular secretions supportive of implantation.
- The endometrium also becomes even thicker and more vascular.
- Endometrium is prepared to nourish a growing embryo if the oocyte is fertilized.
Disorders of the Menstrual Cycle
1 Amenorrhea
- Primary: no menarche by age 15
- Secondary: absence for ≥3 months after established cycles
Causes: PCOS, hyperprolactinemia, thyroid disease, pregnancy.
2 Dysmenorrhea
- Painful menstruation
- Primary (prostaglandin-related)
- Secondary (endometriosis, fibroids)
3 Abnormal Uterine Bleeding (AUB)
- Heavy or irregular bleeding
- PALM-COEIN classification
4.3. Hormonal Profiles Across the Cycle
- Hypothalamus → GnRH → Anterior Pituitary → FSH & LH → Ovary:
◦ Follicle development → Estrogen ↑
◦ LH surge → Ovulation
◦ Corpus luteum → Progesterone ↑
- Uterus:
◦ Estrogen → Endometrial proliferation
◦ Progesterone → Secretory preparation
◦ Hormone withdrawal → Menstruation
5. Cervical Mucus and Fertility
1.1 Types of Cervical Mucus
- Dry phase (post-menstrual)
- Creamy phase (early fertile window)
- Egg-white cervical mucus (EWCM) → peak fertility
- Sticky phase (post-ovulation)
1.2 Fertility Significance
- EWCM: thin, stretchy, alkaline → facilitates sperm survival & transport.
- Post-ovulation mucus → thick and acidic → prevents sperm entry.
1.3 Basal Body Temperature (BBT) and Ovulation
1.3.1 BBT Pattern
- Pre-ovulation: lower temperatures
- After ovulation: progesterone raises BBT by 0.3–0.5°C
- Remains elevated in luteal phase.
1.3.2 Clinical Uses
- Identifies luteal phase defects.
- Confirms ovulation, but does NOT predict it.
1.4 Ovulation Prediction and Fertile Window
1.4.1 Fertile Window
- 6-day period: 5 days before ovulation + ovulation day.
- Greatest fertility:
- Day −2 to Day 0.
1.4.2 Ovulation Prediction Methods
- LH urine surge detectors
- Cervical mucus monitoring
- Ultrasound follicle tracking
- Hormonal blood tests
- BBT charting (retrospective)
6. Factors Affecting Fertility
1.1 Female Factors
- Age (most significant factor)
- Ovulatory disorders (PCOS, thyroid dysfunction)
- Tubal blockage
- Endometriosis
- Uterine abnormalities
1.2 Male Factors
- Low sperm count
- Poor motility or morphology
- Varicocele
- Hormonal disorders
1.3 Lifestyle Influences
- Smoking, alcohol, obesity
- Stress
- Exercise extremes
- Poor diet
- Exposure to environmental toxins
7. Hormonal Regulation of Reproduction
1 Hypothalamic–Pituitary–Gonadal (HPG) Axis
- GnRH → anterior pituitary
- FSH & LH → gonads
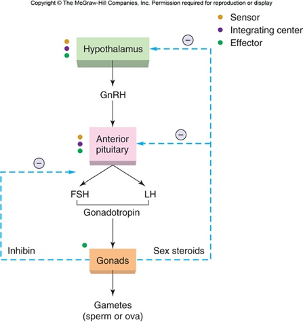
.2 In Males
- LH → Leydig cells → testosterone
- FSH → Sertoli cells → spermatogenesis
- Testosterone & inhibin → negative feedback.
3 In Females
- FSH → follicle growth
- LH → ovulation & corpus luteum
- Estrogen & progesterone → regulate uterus & feedback.
8. Self-Assessment Questions
- Describe the hormonal regulation of spermatogenesis.
- What triggers ovulation?
- Outline the phases of the menstrual cycle.
- Explain the role of LH in both males and females.
- Describe two major functions of progesterone.
- What is capacitation, and why is it necessary?