Chapter 1: Overview of the Endocrine System
| Site: | Newgate University Minna - Elearning Platform |
| Course: | Endocrine and Reproductive System |
| Book: | Chapter 1: Overview of the Endocrine System |
| Printed by: | Guest user |
| Date: | Saturday, 3 January 2026, 10:20 PM |
Description
Learning Objectives:
- Define the endocrine system and describe its major functions.
- Differentiate between endocrine and exocrine glands.
- Explain the role of hormones in maintaining homeostasis
1. Introduction
- The endocrine system is a complex network of cells, tissues, glands and organs that produce, store, and secrete hormones into blood
- Unlike the nervous system (which uses electrical impulses), the endocrine system regulates body functions via chemical messengers transported through the bloodstream.
Key Functions:
- Regulation of growth and development
- Control of metabolism and energy balance
- Maintenance of fluid, electrolyte, and acid–base balance
- Regulation of reproductive processes
- Coordination of the body’s response to stress
2. Hormones and Their Roles
- Hormones are chemical messengers synthesized by specialized glands or cells, released into and travel through the bloodstream to target organs, where they modulate various functions such as growth, metabolism, reproduction, and mood.
- They act on target cells with specific receptors to a particular hormone, influencing:
- Metabolism (e.g., insulin, thyroid hormones)
- Growth, development and aging (e.g., growth hormone, sex steroids)
- Sexual differentiation (sex steroids)
- Reproductive processes (e.g., estrogen, testosterone)
- Behavior: courtship, mating, maternal behavior
- Local effects on specific organs;
o development of the follicle
o uterine changes (menstrual cycle)
o maintenance of pregnancy
o initiation of labor
o milk secretion and ejection
- Homeostasis (e.g., ADH, aldosterone). Major homeostatic variables controlled by the endocrine system:
- Temperature
- Nutrients
- Oxygen
- Pressure
- Ion concentrations
- pH
- Toxic chemicals
3. Types and Mechanisms of Hormonal Action
Learning Objectives:
- Differentiate between peptide, steroid, and amine hormones.
- Describe how hormones act through receptors.
Introduction
The endocrine system plays a vital role in maintaining homeostasis by regulating physiological processes through the secretion of hormones.
Unlike neural signals that act rapidly and locally, hormonal signals are typically slower but have prolonged and widespread effects.
Understanding how hormones function involves two key aspects: the types of hormones based on their chemical structure and origin, and the mechanisms through which they exert their effects on target cells.
The nature of a hormone—whether it's water-soluble or lipid-soluble—determines how it interacts with receptors and initiates a response within the body. These interactions form the foundation of hormonal signaling pathways that influence gene expression, enzyme activity, and cellular function.
Now, let’s explore the types of hormones and the mechanisms of their action in more detail.
3.1. Types of Hormones
- Peptide and Protein Hormones
- consist of multiple amino acids that link to form an amino acid chain.
- Peptide hormones consist of short chains of amino acids, whereas protein hormones are longer polypeptides.
- Both types are synthesized like other body proteins: DNA is transcribed into mRNA, which is translated into an amino acid chain.
- Act on cell surface receptors
- Examples of peptide hormones: insulin, glucagon, ADH
- Examples of protein hormones: GH, FSH
- Steroid hormones
- are derived from the lipid cholesterol.
- Structure: cholesterol derivatives, lipids
- Solubility: lipophilic
- Synthesis: stepwise modification of cholesterol molecule in various intracellular compartments (in the endocrine gland and also in the blood and target tissues)
- Storage: hormones not stored, only precursor (cholesterol) stored
- Secretion: diffusion
- Transport: mostly bound to plasma proteins
- Receptor site: inside of target cell
- Action: direct effects on genes ® production of new proteins
- e.g., cortisol, estrogen, aldosterone.
- Amino Acid Derivatives (Amine hormones)
- are synthesized from the amino acids tryptophan or tyrosine
- Catecholamines (dopamine, epinephrine, and norepinephrine)
- Structure: tyrosine derivative
- Solubility:hydrophilic
- Synthesis: cytosol
- Storage: secretory (chromaffin) granules
- Secretion: exocytosis
- ransport: as a free hormone and bound to plasma proteins
- Receptor site: surface of target cell
- Action: second messenger system
- Thyroid hormones
- Structure: iodinated tyrosine derivative
- Solubility: lipophilic
- Synthesis: extracellular colloid
- Storage: extracellular colloid
- Secretion: endocytosis of colloid
- Transport: mostly bound to plasma proteins
- Receptor site: inside of target cell
- Action: direct effects on genes ® production of new proteins
3.2. Mechanisms of Action
Hormones act by binding to specific receptors and triggering a biological response. The mechanism depends on the hormone type:
1. Recetors
1.1 Membrane Receptor Mechanism (for Water-Soluble Hormones)
- Receptor location: Cell surface.
- Receptor types:
- Direct effects on membrane ion channels (surface receptors)
- Direct activation of intracellular enzymes (surface receptors)
- Activation of G proteins/second messenger system (surface receptors)
- Direct activation of specific genes (intracellular receptors).
Note: A certain receptor type may be present in 100 – 1,000,000 copies on a single cell.
- Mechanism:
- Hormone binds to receptor → activates second messenger system (e.g., cAMP, IP₃/DAG).
- Second messengers amplify the signal inside the cell.
- Examples: Insulin, adrenaline.
1.2. Intracellular Receptor Mechanism (for Lipid-Soluble Hormones)
- Receptor location: Cytoplasm or nucleus.
- Mechanism:
- Hormone enters cell → binds intracellular receptor → hormone-receptor complex binds DNA → regulates gene expression (transcription).
- Examples: Cortisol, thyroid hormones
2. Signal Transduction Pathways
- Once the chemical signal has been detected by the receptor it must be converted, or transduced, to a form that is meaningful to the cell's metabolic machinery.
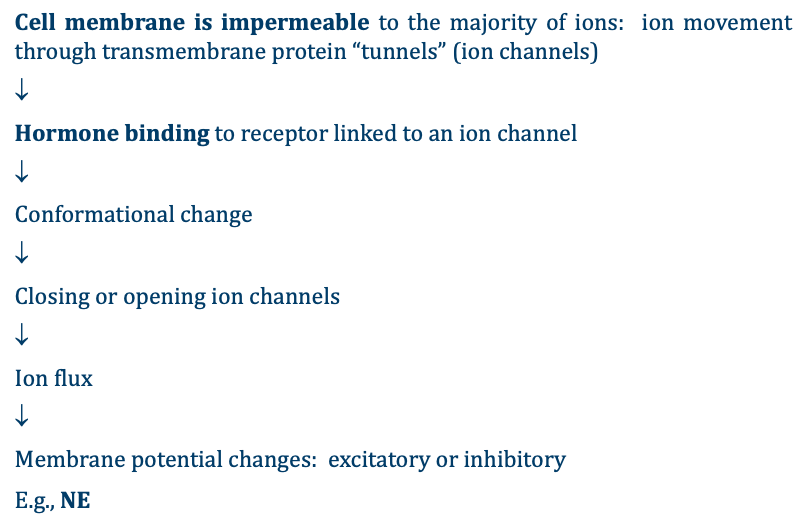
- Binding of hormones to cell surface receptors initiate the closing or opening of ion channels (affecting the permeability of the cell membrane) or initiate a signaling cascade that is carried out by a molecule called a second messenger. In this case, the hormone is called a first messenger.
- Common second messenger systems:
- ion channel‑linked receptors
- cAMP (cyclic AMP) – activates protein kinase A.
- IP₃/DAG (inositol triphosphate/diacylglycerol) – increases intracellular calcium.
- Activation of specific genes
2.1 Pathways Involving Cell Membrane Hormone Receptors
A. ion channel‑linked receptors
B. Enzyme-Linked Receptors (the second messenger pathway)
- Intracellular moiety itself has enzymatic activity or is associated directly with intracellular enzymes → the enzyme produces intra-cellular messengers (called “second messengers”).
- A second messenger in the cytoplasm is required bring about the change in metabolism (the hormone is the first messenger but it never enters the cell).
- The second messenger used by most hormones is cyclic adenosine monophosphate (cAMP).
- In the cAMP second messenger system, a water-soluble hormone binds to its receptor in the cell membrane ((Step 1 in Figure below)
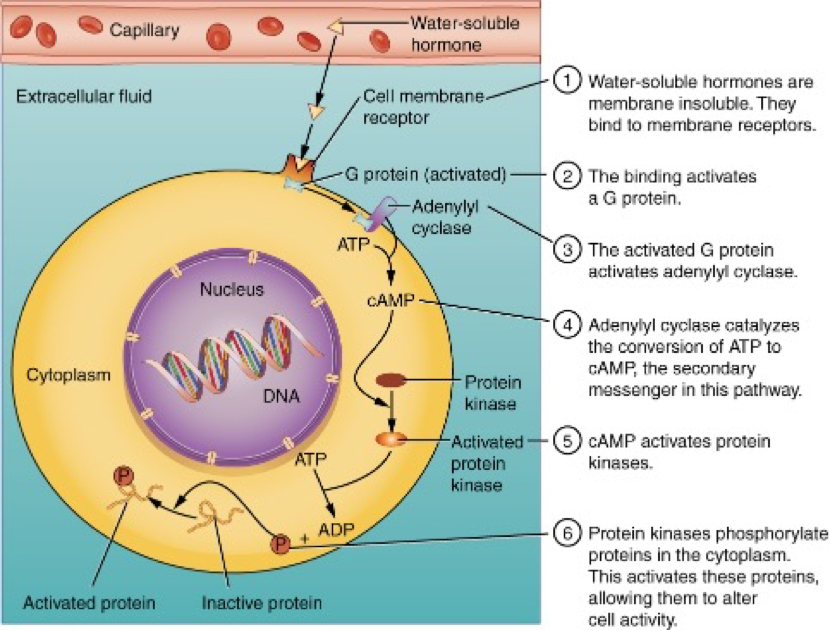
- This receptor is associated with special membrane proteins called G protein, and binding of the hormone activates the G-protein component (Step 2).
- G proteins act as “middlemen” between receptor and second messenger.
- The activated G protein in turn activates an enzyme called adenylyl cyclase, also known as adenylate cyclase (Step 3), which converts adenosine triphosphate (ATP) to cAMP (Step 4).
- As the second messenger, cAMP activates a type of enzyme called a protein kinase that is present in the cytosol (Step 5).
- Activated protein kinases initiate a phosphorylation cascade, in which multiple protein kinases phosphorylate (add a phosphate group to) numerous and various cellular proteins, including other enzymes (Step 6).
- The phosphorylation of cellular proteins can
trigger a wide variety of effects, from nutrient metabolism to the synthesis of
different hormones and other products.
- e.g., cAMP activates protein kinase, which activates phosphorylase kinase, which activates glucose phosphorylase which hydrolyzes glycogen.
- The effects vary according to the type of target cell, the G proteins and kinases involved, and the phosphorylation of proteins
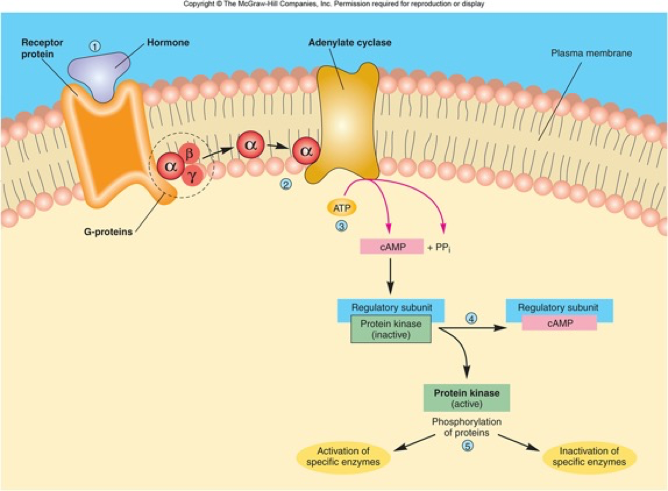
- Examples of hormones that use cAMP as a second messenger include calcitonin, which is important for bone construction and regulating blood calcium levels; glucagon, which plays a role in blood glucose levels; and thyroid-stimulating hormone, which causes the release of T3 and T4 from the thyroid gland.
- Importantly, there are also G proteins that decrease the levels of cAMP in the cell in response to hormone binding. For example, when growth hormone–inhibiting hormone (GHIH), also known as somatostatin, binds to its receptors in the pituitary gland, the level of cAMP decreases, thereby inhibiting the secretion of human growth hormone.
- Not all water-soluble hormones initiate the cAMP second messenger system. One common alternative system uses calcium ions as a second messenger.
- In this system, G proteins activate the enzyme phospholipase C (PLC), which functions similarly to adenylyl cyclase.
- Once activated, PLC cleaves a
membrane-bound phospholipid into two molecules:
- diacylglycerol (DAG) and
- inositol triphosphate (IP3)
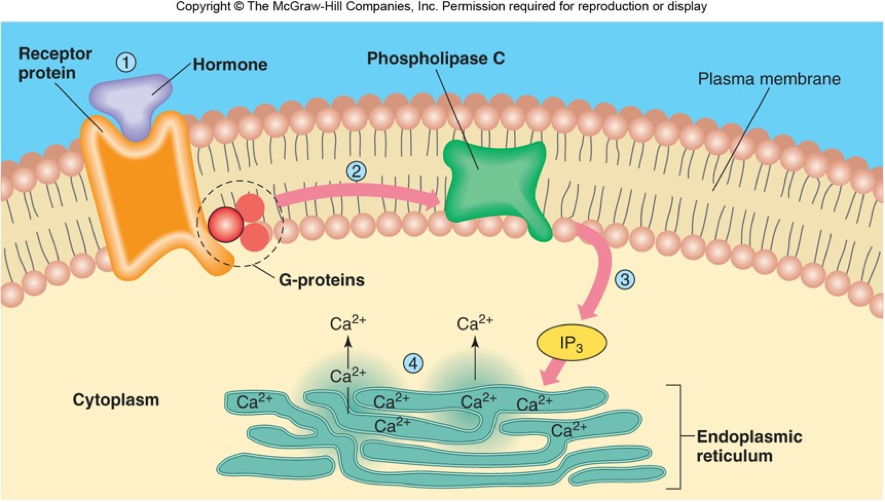
- Like cAMP, DAG activates protein kinases that initiate a phosphorylation cascade. At the same time, IP3 causes calcium ions to be released from storage sites within the cytosol, such as from within the smooth endoplasmic reticulum.
- The calcium ions then act as second messengers in two ways: they can influence enzymatic and other cellular activities directly, or they can bind to calcium-binding proteins, the most common of which is calmodulin.
- Upon binding calcium, calmodulin is able to modulate protein kinase within the cell.
- Examples of hormones that use calcium ions as a second messenger system include angiotensin II, which helps regulate blood pressure through vasoconstriction, and growth hormone–releasing hormone (GHRH), which causes the pituitary gland to release growth hormones.
2.2 Pathways Involving Intracellular Hormone Receptors (Direct gene activation)
§ These hormones are mostly synthesized from cholesterol. These include hormones for sex (estrogen, progesterone, testerone), thyroid and renal (aldosterone) function.
§ These are produced in one cell, then are released into the blood, circulate to all cells, and then permeate across the plasma membrane (due to their lipid solubility) to bind to receptors in the cytosol or nucleus (see step 1 and 2 in Fig below)

- § After binding to the home binding
domain on the receptor, the hormone + receptor complextranslocate to
the nucleus and bind to a
particular sequence of DNA (hormone response element or HRE) in a gene,
which then becomes activated DNA (step 3).
- HRE sites of specific genes, e.g., estrogen-response element; progesterone-response element; etc
- For both steroid and thyroid hormones, binding of the hormone-receptor complex with DNA triggers transcription of a target gene to mRNA (step 4), which moves to the cytosol where it directs protein synthesis by ribosomes (step 5).
- Example
- Low blood [Na] triggers cells in the adrenal cortex to release aldosterone into the blood stream.
- This steroid hormone then circulates throughout the body and binds to receptors in the cytosol of cells in the kidney and gastrointestinal tract.
- The receptor + aldosterone complex moves into the nucleus, where it activates two genes, one for the Na/K-pump and a second for a Na channel.
- These new proteins are inserted into the plasma membranes of the GI and renal cells, leading to increased entry of Na into the cells (through the channels) and increased pumping of Na out of the cells into the blood stream (on the Na/K-pump).
- This increases uptake of Na from the gut and increases Na retention by the kidneys, which increases blood [Na], returning the body to the correct [Na]
- Due to the fact that all this takes time and proteins are produced, steroid hormones generally are longer acting, both in terms of the time it takes to activate the changes in cell functions and also in terms of how long the new protein will act: over hours or even days.
- The final step is the desired metabolic response.
- The response may include the stimulation of protein synthesis, activation or deactivation of enzymes, alteration in the permeability of the cell membrane, altered rates of mitosis and cell growth, and stimulation of the secretion of products.
- Moreover, a single hormone may be capable of inducing different responses in a given cell.
Cellular Response to Hormones:
3.3. Receptor Types
1. Membrane Receptor Mechanism (for Water-Soluble Hormones)
- Receptor location: Cell surface.
- Receptor types:
- Direct effects on membrane ion channels (surface receptors)
- Direct activation of intracellular enzymes (surface receptors)
- Activation of G proteins/second messenger system (surface receptors)
- Direct activation of specific genes (intracellular receptors).
Note: A certain receptor type may be present in 100 – 1,000,000 copies on a single cell.
- Mechanism:
- Hormone binds to receptor → activates second messenger system (e.g., cAMP, IP₃/DAG).
- Second messengers amplify the signal inside the cell.
- Examples: Insulin, adrenaline.
2. Intracellular Receptor Mechanism (for Lipid-Soluble Hormones)
- Receptor location: Cytoplasm or nucleus.
- Mechanism:
- Hormone enters cell → binds intracellular receptor → hormone-receptor complex binds DNA → regulates gene expression (transcription).
- Examples: Cortisol, thyroid hormones
4. Mechanisms of Hormone Regulation and Feedback Loops
Learning Objectives:
- Explain negative and positive feedback in hormone control.
- Give examples of feedback loops in the endocrine system.
Overview:
§ To prevent abnormal hormone levels and a potential disease state, hormone levels must be tightly controlled.
§ The body maintains this control by balancing hormone production and degradation. Feedback loops govern the initiation and maintenance of most hormone secretion in response to various stimuli.
§ Hormone secretion is regulated mainly by feedback mechanisms.
§ Feedback loop is a regulatory mechanism in which the output of a process influences its own activity.
4.1. Negative feedback
- The more common method of hormone regulation is the negative feedback loop.
- Negative feedback is characterized by the inhibition of further secretion of a hormone in response to adequate levels of that hormone.
- This allows blood levels of the hormone to be regulated within a narrow range.
- An example of a negative feedback loop is the release of thyroid hormones from the thyroid glands, as directed by the hypothalamus and pituitary gland (see Fig below)
As thyroxine concentrations in the blood rise, the hypothalamus and pituitary gland reduce their signaling to the thyroid glands to prevent additional thyroxine secretion.

4.2. Positive feedback
- Positive feedback loops are characterized by the release of additional hormone in response to an original hormone release.
- Thus, positive feedback enhances change.
- Example: Oxytocin during childbirth → uterine contractions → more oxytocin → stronger contractions.
- The initial release of oxytocin begins to signal the uterine muscles to contract, which pushes the fetus toward the cervix, causing it to stretch. This, in turn, signals the pituitary gland to release more oxytocin, causing labor contractions to intensify. The release of oxytocin decreases after the birth of the child.
5. Major Endocrine Glands
Learning Objectives:
- Identify the major endocrine glands.
- Summarize the hormones they produce.
Endocrine Glands
- secretory cells
- connective tissue
- blood vessels
- no duct
- innervation and vascularization (fenestrated capillaries)
- One gland can produce several types of hormones same hormone can be produced by various glands.
- Endocrine glands differ from Exocrine glands (exo = “outside”) in that exocrine glands secrete enzymes, waste products, etc. NOT hormones
- Exocrine glands do NOT into the bloodstream
- several organs have both endocrine and exocrine glands (e.g., pancreas, gut)
|
Gland |
Major Hormones |
Key Functions |
|
Hypothalamus |
Releasing/inhibiting hormones |
Controls pituitary |
|
Pituitary |
GH, ACTH, TSH, LH, FSH, ADH, Oxytocin |
Master gland |
|
Thyroid |
T3, T4, Calcitonin |
Regulates metabolism, calcium |
|
Adrenal |
Cortisol, Aldosterone, Adrenaline |
Stress response, metabolism, fluid balance |
|
Pancreatic Islets |
Insulin, Glucagon |
Blood glucose regulation |