Hypothalamus and Pituitary Gland
Learning Objectives:
- Describe the location and anatomy of the hypothalamus and pituitary.
- Explain the functional relationship between the two structures.
2. Anterior Pituitary (Adenohypophysis)
Introduction
- The anterior pituitary has no direct neural connection with the hypothalamus.
- Instead, it is regulated by hypothalamic releasing and inhibiting hormones transported through the Hypothalamo–Hypophyseal Portal veins or system (see figure in unit 1.4).
- This unconventional vascular connection between the hypothalamus and posterior pituitary ensures that minute quantities of hypothalamic hormones are carried in a concentrated form directly to their target cells in the anterior pituitary, and are not diluted out in the systemic circulation.
Embryology & Structure
- Derived from Rathke’s pouch, an ectodermal outgrowth of the primitive oral cavity.
- Forms about 75% of the pituitary gland.
- Subdivisions:
- Pars distalis (main secretory portion)
- Pars tuberalis (wraps around infundibulum)
- Pars intermedia (rudimentary in humans)
Hypothalamo–Hypophyseal Portal System
- Hypothalamic neurons release hormones into primary capillary plexus in the median eminence.
- Hormones travel via portal veins to secondary capillary plexus in the anterior pituitary.
- Target secretory cells in the adenohypophysis, stimulating or inhibiting hormone secretion.
Hypothalamic Control of the Anterior Pituitary
The anterior pituitary has no direct neural connection with the hypothalamus. Instead, it is regulated by hypothalamic releasing and inhibiting hormones transported through the hypophyseal portal system (see fig in section 1.4 and below)
- Arcuate nucleus (Tuberal region): major source of releasing/inhibiting hormones
- Paraventricular nucleus: secretes corticotropin-releasing hormone (CRH), thyrotropin-releasing hormone (TRH), and somatostatin
- Preoptic area: secretes gonadotropin-releasing hormone (GnRH)
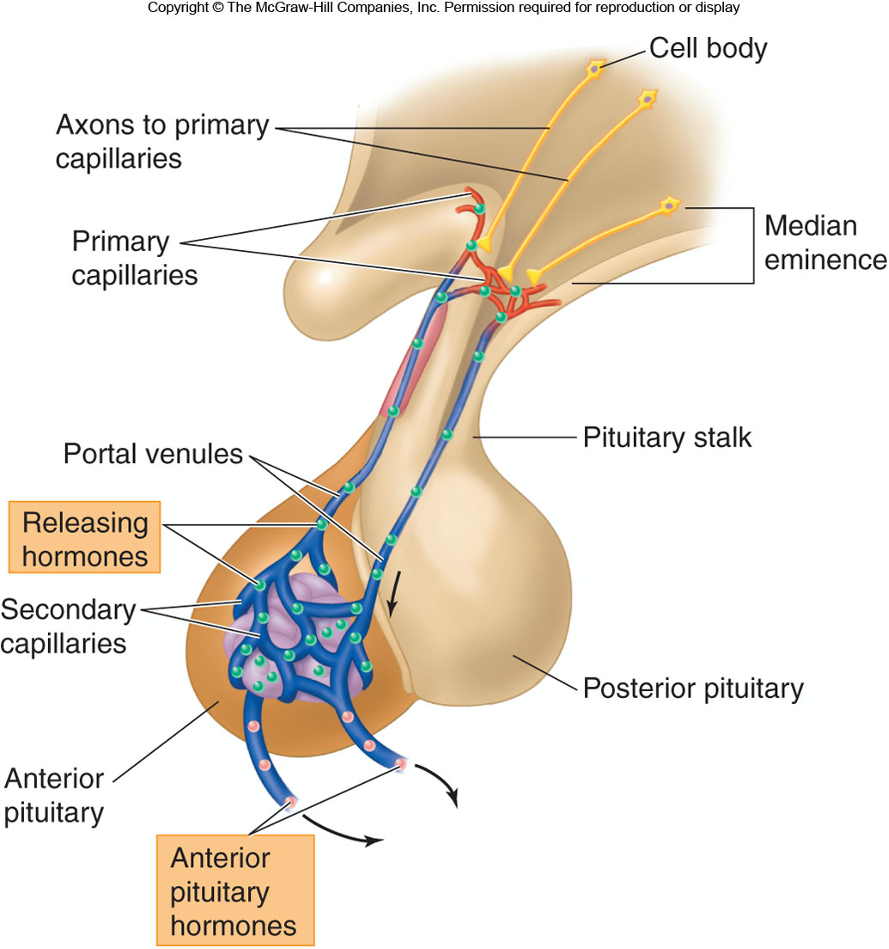
- The anterior pituitary is controlled via releasing and inhibiting hormones produced in the hypothalamus. and
- These hormones are transported to the Anterior Pituitary through the hypothalamo-hypophyseal portal system.
This is the only case in which hormones released into the blood do not go to the entire body
|
Hypothalamic Hormone |
Effect on Anterior Pituitary |
|
Corticotropin-releasing hormone (CRH) |
Stimulate secretion of adrenocorticotropic Hormones (ACTH) |
|
Gonadotropin-releasing hormone (GRH) |
Stimulate secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) |
|
Prolactin-inhibiting hormone (PIH) |
Inhibits prolactin secretion |
|
Somatostatin |
Inhibits secretion of growth hormone |
|
Thyrotropin-releasing hormone (TRH) |
Stimulates secretion of thyroid-stimulating hormone (TSH) |
|
Growth hormone−releasing hormone (GHRH) |
Stimulates growth hormone secretion |
Growth hormone (GH)
Thyroid-stimulating hormone (TSH)
Adrenocorticotropic hormone (ACTH)
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LH)
Prolactin
|
Hormone |
Source Cells |
Target Organ(s) |
Main Function(s) |
|
GH (Growth Hormone) |
Somatotrophs |
Liver, bone, muscle |
Stimulates growth, protein synthesis, IGF-1 secretion |
|
TSH (Thyroid-Stimulating Hormone) |
Thyrotrophs |
Thyroid gland |
Stimulates T₃ and T₄ secretion |
|
ACTH (Adrenocorticotropic Hormone) |
Corticotrophs |
Adrenal cortex |
Stimulates cortisol production |
|
LH (Luteinizing Hormone) |
Gonadotrophs |
Gonads |
Ovulation, corpus luteum, testosterone secretion |
|
FSH (Follicle-Stimulating Hormone) |
Gonadotrophs |
Gonads |
Follicular growth, spermatogenesis |
|
PRL (Prolactin) |
Lactotrophs |
Mammary glands |
Milk production |
|
MSH (Melanocyte-Stimulating Hormone) |
Pars intermedia (rudimentary) |
Skin melanocytes |
Pigmentation (minor role in humans) |
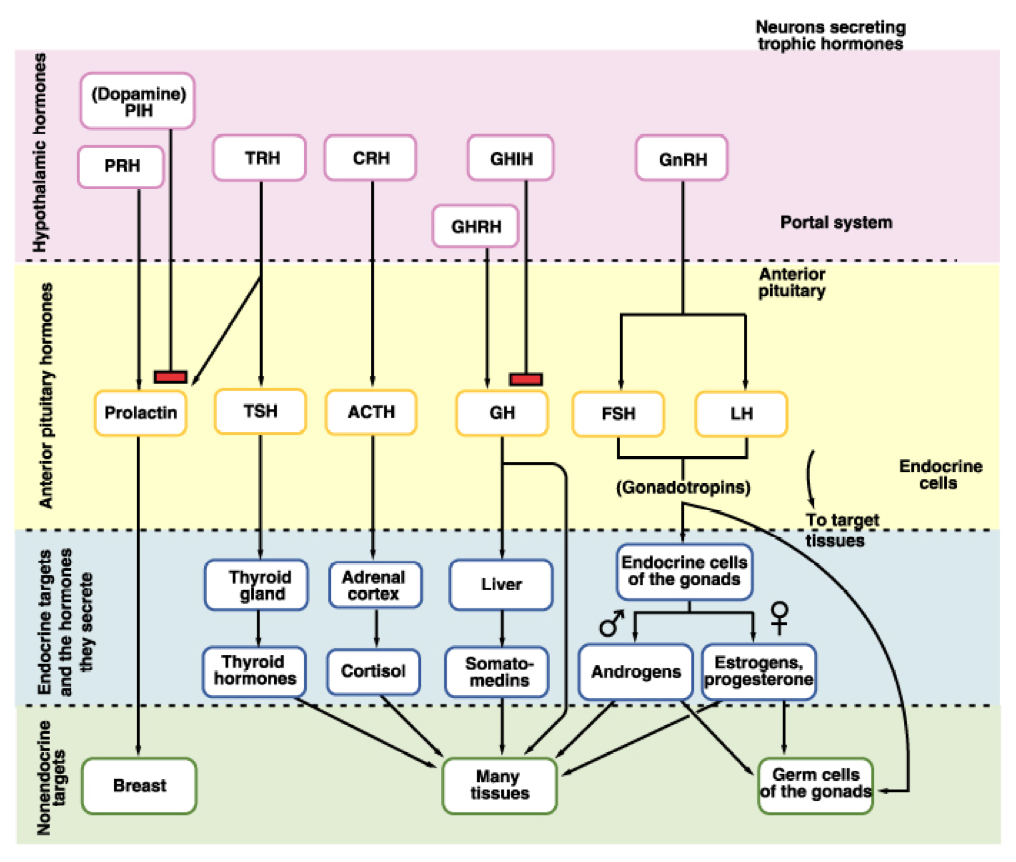
GH → Liver → Growth via IGF
ACTH → Adrenal Cortex → Cortisol release
TSH → Thyroid → Thyroid hormones (T3, T4)
FSH/LH → Gonads → Gametogenesis & sex hormones
PRL → Mammary glands → Milk production and growth of mammary glands
Feedback Control of Anterior Pituitary
Release of tropic hormones is controlled by the hypothalamus which is in turn controlled by the activity of the target glands.
Example: Hypothalamus-Pit-Thyroid Axis
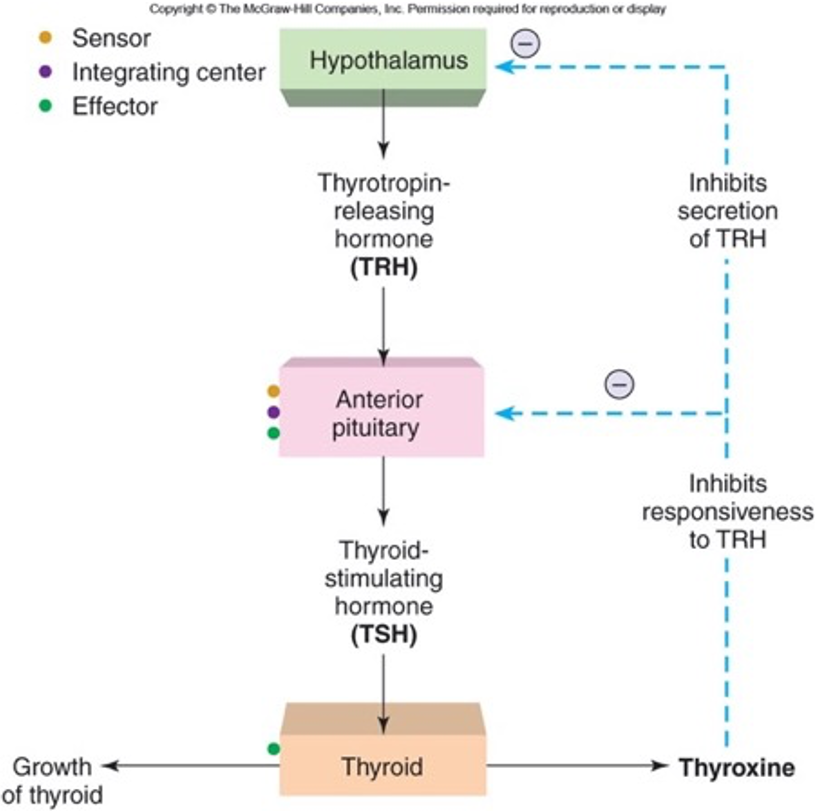
Low levels of thyroxin in the blood stimulate the hypothalamus to secrete thyroid stimulating hormone releasing hormone into the hypophyseal portal system.
The portal system delivers this hormone to the secretory cells of the anterior pituitary which secrete thyroid stimulating hormone (TSH) into general systemic circulation in response.
The blood carries the TSH hormone to the thyroid gland which has cells with receptor proteins for TSH hormone.
Thyroid cells secrete thyroxin into the blood which carries it throughout the body.
Target cells all over the body respond by increasing oxidative RNA synthesis and metabolism.
Cells of the hypothalamus, however, respond to the elevated thyroxin levels by decreasing their production of thyroid stimulating hormone releasing hormone.
This causes the anterior pituitary to decrease production of TSH which in turn causes the thyroid to decrease production of thyroxin.
Blood levels of thyroxin decrease.
The final product regulates secretion of pituitary hormones.
Inhibition can occur at the hypothalamus or pituitary gland level, inhibiting secretion of releasing or stimulating hormones respectively.
Key Points:
- Secretion of anterior pituitary hormones is under hypothalamic regulation except prolactin, which is mainly inhibited by dopamine.
- Blood supply via superior hypophyseal arteries (from internal carotid), forming the portal circulation.

