Lecture Notes on Male and Female Reproductive Physiology
2. Male Reproductive Anatomy
2.1 External Genitalia
- Penis: urethra, glans, erectile tissue (corpora cavernosa & corpus spongiosum).
- Scrotum: houses testes; temperature regulation (≈34°C).
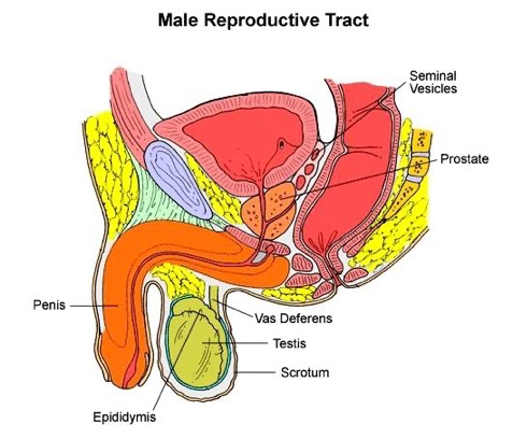
2.2 Internal Reproductive Structures
- Testes: seminiferous tubules (sperm production), Leydig cells (testosterone).
- Epididymis: sperm maturation & storage.
- Vas deferens: transport of sperm.
- Accessory glands:
- Seminal vesicles (60% semen volume)
- Prostate gland (enzymes, citrate)
- Bulbourethral glands (lubrication)
2.3 Blood-Testis Barrier
- Formed by tight junctions of Sertoli cells.
- Protects germ cells from immune system.
- Maintains specialized microenvironment for spermatogenesis.
2.4: Male Sexual Response
- The main phases of the male sexual response are:
- erection
- emission and
- ejaculation.
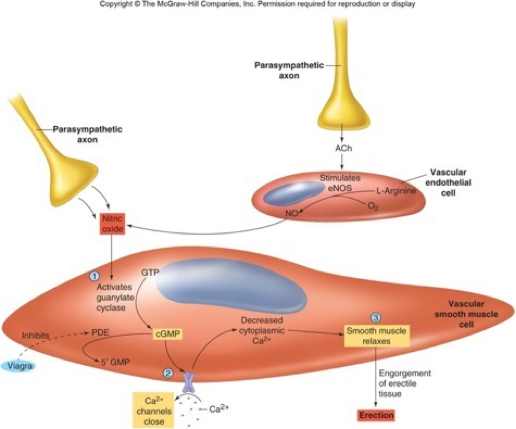
2.4.1 Erection
- Erection results from engorgement of the erectile bodies with blood.
- Can occur due to conscious sexual thought
- hypothalamus sacral region of the spinal cord penis), or
- sensory stimulation: penis spinal cord penis
- Parasympathetic (S2–S4) → nitric oxide release → vasodilation → erection.
- Activation of parasympathetic nerves to the penis increases local nitric oxide (NO) release
- NO results in increased blood flow into and engorgement of the erectile tissues of the penis.
- This results in an erection, which allows the penis to penetrate the vagina.
- Inhibited by stress, sympathetic activity.
2.4.2 Emission and Ejaculation
- Emission is the movement of semen into the urethra
- Ejaculation is the forceful expulsion of semen from the urethra due to rhythmic contraction of pelvic muscles.
- Both are under sympathetic nervous system control.
- Contraction of smooth muscles in the tubules, seminal vesicle, prostate, and muscles at base of penis is involved in ejaculation.
- Detumescence
- erection subsides: sympathetic constricts arterioles
- latent period: new ejaculation not possible (min-hrs)
2.5 Semen
§ Semen, also known as seminal fluid or ejaculate, is the whitish-gray fluid released by males during sexual climax (ejaculation).
§ These fluids originate from the testicles, seminal vesicles, and prostate gland.
§ Function:
o Semen's primary role is to carry sperm to the female reproductive tract for fertilization.
o It also provides a nutrient-rich environment for sperm survival and motility.
§ 2-5ml/ejaculation contains;
o 60% seminal fluid from seminal vesicles (fructose, amino acids, citric acid, phosphorus, potassium, and prostaglandins)
o 30% prostatic fluid from the prostate gland (citric acid, acid phosphatase, calcium, sodium, zinc, potassium, enzymes, and fibrolysin);
o 10% testicular fluid from testes (50-300million sperm/ml; less than 60 million total = sterile).
§ Characteristics
o Appearance: Typically grey-opalescent, it initially clots and then liquefies over time.
o Volume: The average volume is about 1 to 5 milliliters per ejaculate.
o Smell/Taste: It can have a chlorine-like or slightly fishy odor and a slightly sweet taste due to fructose.
o pH: It is slightly alkaline, with a pH range of 7.2 to 7.8, which helps protect sperm in the acidic environment of the vagina.
§ Everyday a healthy adult male produce about 400 million sperm.
2.6 Clinical Note
- Fertility and sexual function decline with age due to declining levels of sex hormones
- age 50 men go through a period of physical and psychological change = climacteric
- older men are also more likely to father children with autism, epilepsy or schizophrenia
- A sperm count < 20 million/ml semen is called oligospermia and is considered less fertile. May be caused by heat, drugs, or anabolic steroids
- Erectile dysfunction: vascular, neurogenic, endocrine, or psychogenic causes.

