Lecture Notes
Completion requirements
4. Lactogenesis (Milk Production)
4.1 Phases of Lactogenesis
- Lactogenesis I (mid-pregnancy to early postpartum)
- Milk components begin forming (colostrum)
- Progesterone inhibits full secretion
- Lactogenesis II (day 2–3 postpartum)
- Triggered by sharp fall in progesterone while prolactin remains high
- Sudden increase in milk volume (“milk coming in”)
- Lactogenesis III (maintenance phase)
- Controlled mainly by infant suckling and milk removal
- Supply-demand regulated
4.2 Hormonal Control
- Prolactin (anterior pituitary)
- Stimulates milk synthesis
- Levels rise with suckling stimulus
- Oxytocin (posterior pituitary)
- Causes alveolar contraction: milk ejection reflex
- Estrogen and Progesterone
- hPL, cortisol, insulin, thyroid hormones
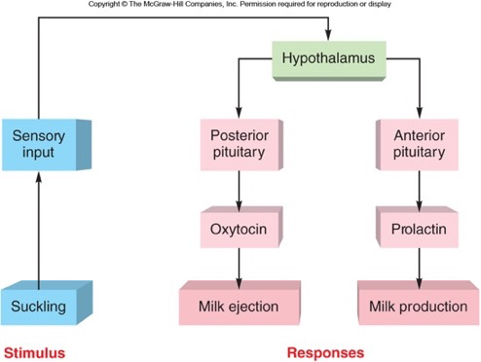
4.3: Milk Ejection (Let-Down Reflex)
1 Oxytocin Reflex
- Triggered by suckling or emotional cues (hearing baby cry)
- Oxytocin causes contraction of myoepithelial cells around alveoli
- Milk is propelled into ducts and nipple
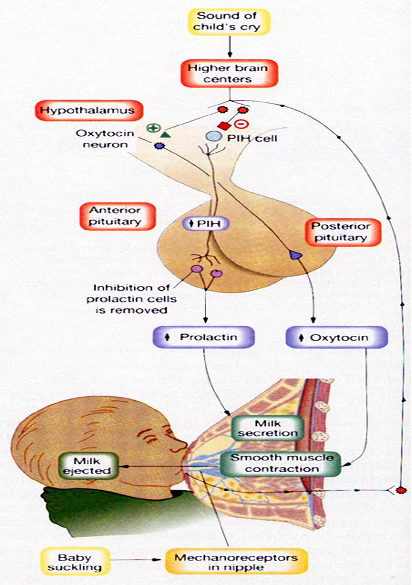
4.4 Factors Influencing Let-Down
- Enhancers: relaxation, warmth, confidence
- Inhibitors: stress, pain, anxiety
4.5: Composition of Breast Milk
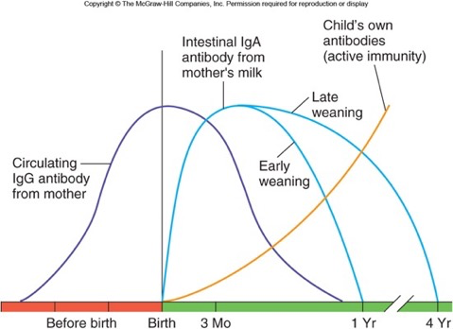
1 Colostrum
- Produced first 2–5 days
- Rich in:
- Immunoglobulin A (IgA)
- Lactoferrin
- Leukocytes
- Growth factors
- Low volume but highly concentrated
- Critical for immune protection and gut maturation
2 Transitional Milk (Day 5–14)
- Higher calories and fat
- Increasing lactose and volume
3 Mature Milk (After 2 Weeks)
- Foremilk: watery, quenches thirst
- Hindmilk: rich in fat, promotes growth
4 Nutritional Components
- Carbohydrates: lactose
- Proteins: casein, whey proteins
- Fats: long-chain fatty acids
- Vitamins and minerals
- Enzymes (lipase, amylase)
4.5 Immunological Components
- IgA
- Lactoferrin
- Lysozyme
- Oligosaccharides (prebiotics)
- Live immune cells
4.6: Lactational Amenorrhea
1 Mechanism
- High prolactin suppresses GnRH
- Low FSH and LH → inhibits ovulation
- Natural but variable contraceptive effect
2 Lactational Amenorrhea Method (LAM)
- Effective (>98%) if:
- Baby is exclusively breastfed
- Mother is within 6 months postpartum
- Menstruation has not resumed
4.8: Clinical Aspects of Lactation
1 Common Issues
- Engorgement
- Blocked ducts
- Mastitis
- Nipple soreness or fissures
- Poor latch
- Inadequate milk supply
2 Management Principles
- Frequent breastfeeding
- Correct breastfeeding technique
- Warm compresses
- Antibiotics for mastitis if required
- Lactation counseling
4.8: Infant Benefits of Breastfeeding
1 Nutritional Benefits
- Ideal composition for growth
- Easily digestible
2 Immunological Protection
- Lower risk of infections
- Gut protection and microbiome formation
3 Long-Term Outcomes
- Improved cognitive development
- Lower risk of obesity and metabolic disorders
4.9: Maternal Benefits of Breastfeeding
Short-Term Benefits
- Faster uterine involution
- Reduced postpartum bleeding
- Natural contraception (LAM)
Long-Term Benefits
- Reduced breast and ovarian cancer risk
- Lower risk of type 2 diabetes
- Emotional bonding
4.10: Summary
- Lactation is hormonally regulated by prolactin (milk production) and oxytocin (milk ejection).
- Breast milk composition changes from colostrum → transitional → mature milk.
- Breastfeeding benefits both infant and mother.
- Postpartum maternal physiology includes uterine involution, fluid shifts, and hormonal changes.
- Lactational amenorrhea provides temporary natural contraception.
- Clinical issues require prompt management and support.

